The political economy of corporatism in medicine: Self-regulation or cartel management?
When Pathology and Laboratory Medicine Becomes a Commodity and Health Care Becomes Both Its Customer and Owner
Fa més de tres dècades que en Peter Zweifel i en Rein Eichenberger van escriure un article significatiu sobre el corporativisme en medicina. En concret es fixaven en una qüestió que passa sovint desapercebuda, la delegació de les tasques regulatòries del govern en les organitzacions mèdiques. Fonamentalment, se centrava en les qüestions d'accés a la professió, nombre de professionals en formació sanitària especialitzada i tipus, o la definició de les especialitats. Deia que tot plegat, en els set països que analitzava, havia donat lloc a una densitat de metges (número de metges per càpita)que era diferent segons el nivell de corporativisme en medicina del país. I després afegia que un fort corporativisme reduïa l'impacte negatiu d'una major oferta de professionals en els ingressos econòmics dels metges.
Agafem un exempre recent. La setmana passada es va crear una nova especialitat que en diuen de Laboratori Clínic, a partir de la fusió de dues especialitats existents, Anàlisis Clíniques i Bioquímica. L'argumentació és magnífica,
La evolución tecnológica va a seguir condicionando este tipo de estructuras organizativas en los centros sanitarios de mayor tamaño, donde se forman la mayoría de los especialistas, pero también va a condicionar el trabajo en centros comarcales, que van a requerir de especialistas más polivalentes.
El trabajo conjunto, en cualquiera de estas estructuras organizativas, no solo evita la fragmentación de la atención y el conocimiento, si no que genera el efecto contrario, unificando la atención a los y las pacientes e integrando conocimientos.
Con este proyecto, se persigue de esta forma mejorar la formación de los especialistas en Ciencias de la Salud, a la vez que se facilita la gestión de los recursos humanos en salud.
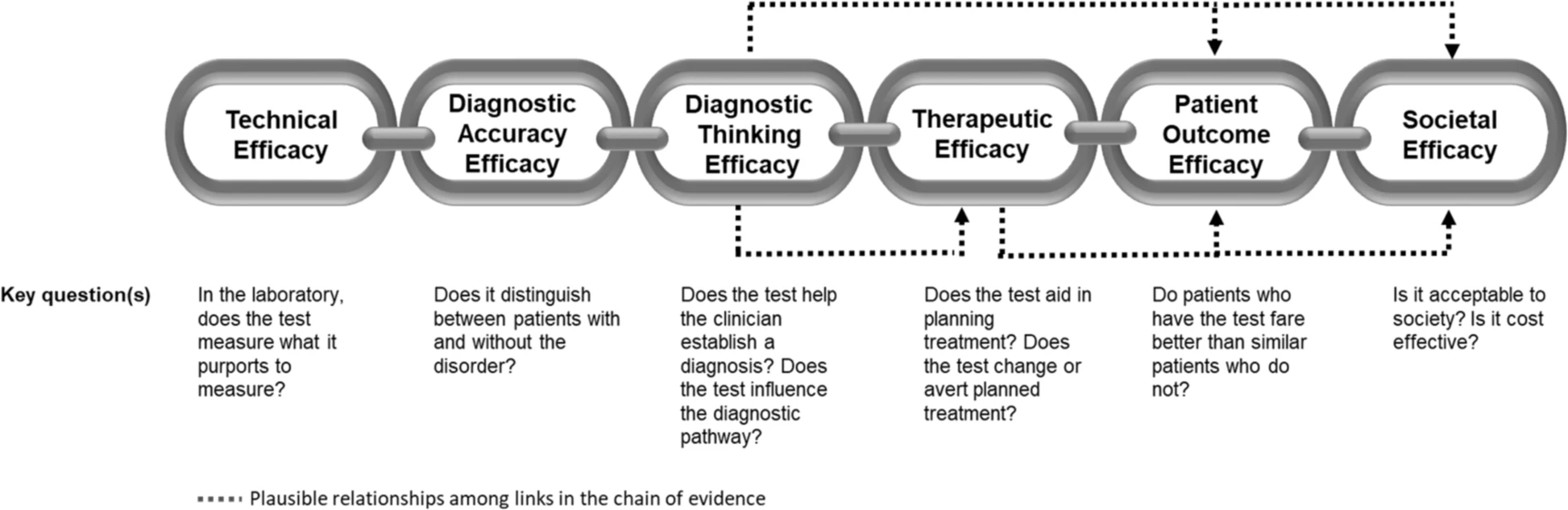
La tecnologia condiciona l'organització, punt. L'organització acaba rendint-se a la tecnologia. Però si és així, jo em pregunto per què han mantingut l'Anatomia Patològica al marge? L'anàlisi d'ADN circulant fa confluir també amb l'activitat dels patòlegs. Molts països ja ho han fet. I la fusió i redefinició d'especialitats hauria de continuar assenyadament en molts més casos. Ara bé, dir-ne Laboratorio Clínico és un disbarat per als annals de la història de la medicina. Aquest nom no és una especialitat, una disciplina mèdica, és tant sols un tros d'un edifici de l'hospital o d'una organització en general. La disciplina és la Medicina de Laboratori, el nom convencional europeu per aquesta especialitat. I quin hauria de ser el model d'especialitat i d'organització? . Doncs com a exemple mirar cap al Canadà i cap Alberta en particular donaria pistes del que cal fer. Aquesta taula ho resumeix:

Segurament a data d'avui caldria reescriure l'article de Zweifel i redefinir els papers de cadascú. Han passat moltes coses d'ençà d'aleshores. Però n'hi ha una que roman, l'escassetat de metges. I la pregunta que molts es fan, és per què hi ha escassetat?. Doncs que mirin qui decideix les places de forma efectiva, qui accepta que hi hagi determinada oferta i la resposta serà immediata. Molts diuen que el govern no ha planificat, i és cert. Però encara que hagués planificat té delegada la regulació parcialment en
comissions de les especialitats i en la comissió nacional, així com els degans d'universitat, i també cal recordar-ho, hi tenim les decisions arbitràries de les comunitats autònomes. Unes comisions que en diuen assessores però que a la pràctica exerceixen com a lobby d'influència determinant i decisor. Mentre no es modifiqui el corporativisme i l'estructura legal que facilita la delegació de la regulació que deia Zweifel no hi haurà solució als problemes d'accés i qualitat a l'assistència per part de la població.
Fa cinc anys
Eric Topol va fer un informe per al NHS sobre com la digitalització modificaria la tasca dels professionals de la salut al NHS. Allà no l'hi han fet massa cas, però aquí ni tant sols hi ha un informe.
Resum. Hi ha un embut perfectament dissenyat. No hi ha el nombre ni tipus de metges que es necessiten per afrontar les tasques i disposar d'un accés digne als serveis. Tot el que observem com a resultat no és un error de planificació del nombre de metges, és exactament tal com s'ha previst que sigui, possiblement per deixadesa.
Hospital de la Santa Creu

.jpg)