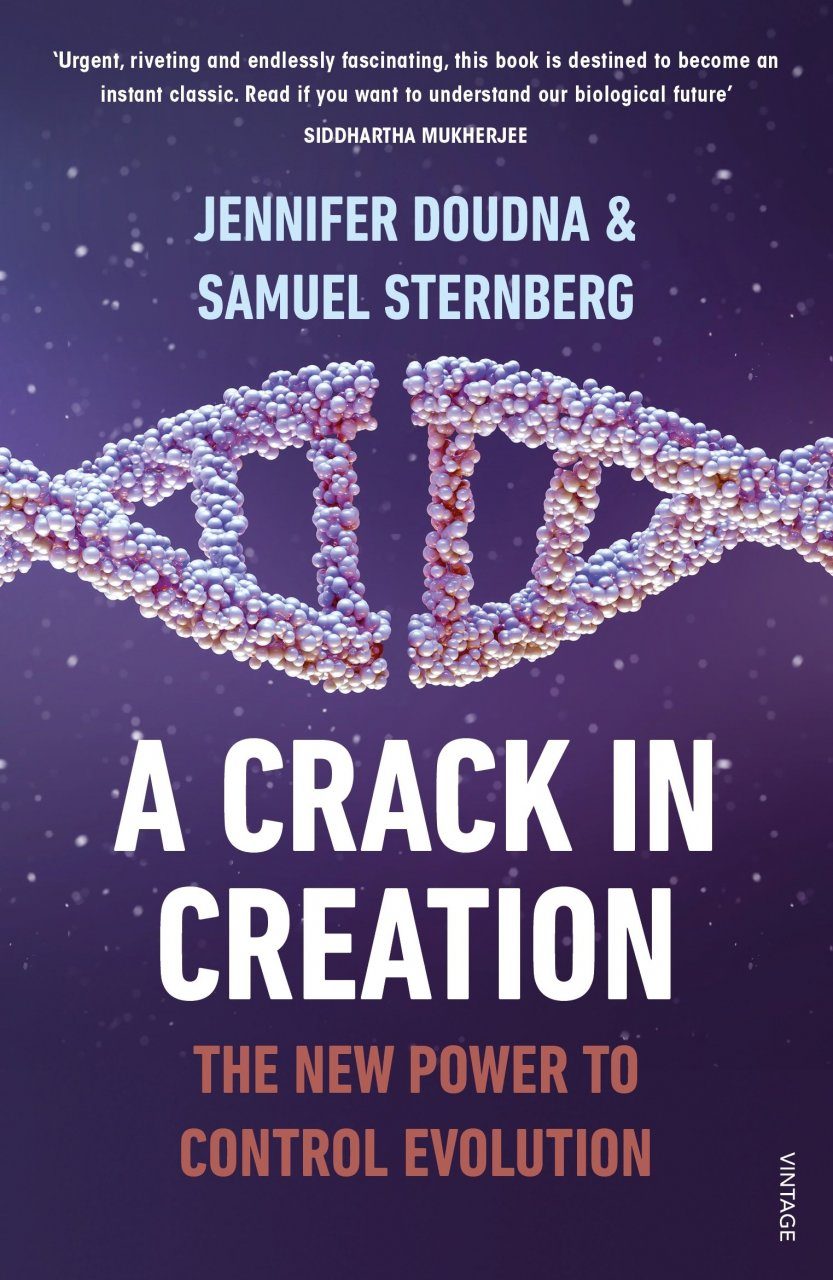
A new publication by Fundació Grifols highlights the potential constraints to genomic editing. It is a good moment to have a look at it. Savador Macip says:
Los peligros, pues, son muchos, tantos como las cosas buenas que la edición genética nos puede aportar. De alguna forma, recuerda la energía nuclear. Descubrir los secretos del átomo nos ha permitido acceder a una cantidad inimaginable de energía, que usamos diariamente, pero que se debe regular de una forma muy precisa para evitar accidentes terribles y contaminaciones no deseadas. Y, lo que es más peligroso aún, la misma información sirve para fabricar una de las armas más mortíferas que conocemos, capaz incluso de destruir el planeta. A otra escala, CRISPR/Cas9 podría tener efectos parecidos.
La ciencia no se detiene, siempre continúa avanzando, y la sociedad corre el peligro de quedarse atrás. Por ello es importante que los debates sobre hacia dónde queremos ir empiecen cuanto antes mejor y que en ellos participe una muestra amplia de la población, no solo los científicos. Para conseguirlo es necesario que el máximo número posible de gente esté bien informada acerca de los avances más recientes, que entienda su alcance y sus implicaciones y que haga el esfuerzo de contribuir en los debates. A la vez, los científicos deben salir a explicar qué está pasando en sus laboratorios y los políticos deben proporcionar plataformas necesarias para estas discusiones. Solo así nos aseguraremos de que estos descubrimientos son usadosA must read.
Side effects, a good film to watch