Valuing Health in Practice: Priorities, QALYs, and Choice
Malgrat la meva posició eclèctica sobre la qüestió, un repàs a aquest llibre és convenient.
Resum amb IA.
El llibre "Valuing Health in Practice: Priorities, QALYs, and Choice" de Douglas McCulloch explora la complexitat de la valoració de la salut i la presa de decisions en el sector sanitari, especialment davant l'escassetat de recursos.
Tema Central: Valoració de la Salut i Escassetat McCulloch argumenta que, donada l'escassetat de recursos, les decisions en el sector sanitari impliquen inevitablement una valoració de la salut. L'objectiu és aconseguir el màxim impacte possible en la salut amb els recursos disponibles. El llibre se centra principalment en el Quality-Adjusted Life Year (QALY) com a mesura fonamental per a aquesta valoració.
Capítol 1: Prioritats, QALYs i Elecció El capítol comença amb un exemple real d'un pacient en llista d'espera que va rebre una cirurgia de bypass després que un investigador notés el seu estat de salut crític. Aquest cas il·lustra la necessitat d'avaluar la qualitat de vida i les expectatives de supervivència de manera rutinària.
El llibre explora tres mètodes principals per a la presa de decisions en salut:
- Programmed Budgeting and Marginal Analysis (PBMA): Un enfocament no prescriptiu que implica identificar programes, establir pressupostos, decidir canvis (introduir, expandir, contractar serveis), mesurar costos i beneficis d'aquests canvis i fer recomanacions basades en el judici.
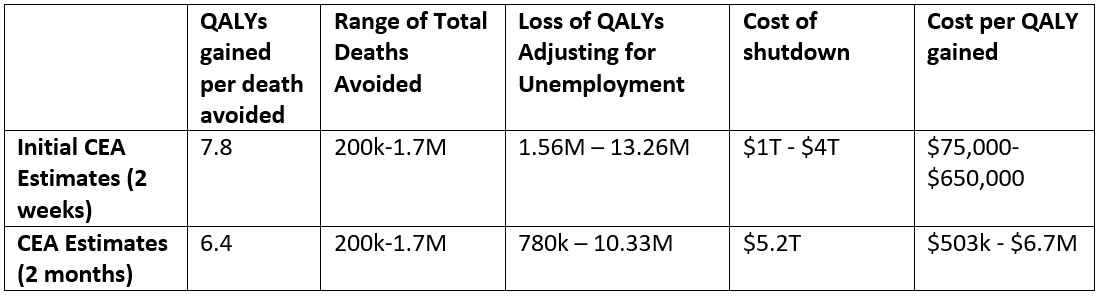
- Cost-Effectiveness Analysis (CEA): Un model que compara alternatives en termes de cost per unitat de resultat (p. ex., cost per QALY o per any de supervivència) amb l'objectiu de maximitzar l'impacte en la salut. Les anàlisis de cost-eficàcia que utilitzen QALYs com a mesura de resultat s'anomenen "Anàlisis de Cost-Utilitat". S'emfatitza la importància de les suposicions, la distinció entre costos mitjans i marginals, i la necessitat d'especificar clarament les intervencions, costos i resultats rellevants, a més de tenir en compte les incerteses mitjançant l'anàlisi de sensibilitat.
- Cost-Benefit Analysis (CBA): La tècnica preferida pels economistes per avaluar projectes des d'un punt de vista comunitari, aplicant l'economia del benestar. Implica mesurar tots els efectes (positius i negatius) en el benestar individual en termes monetaris. Tot i la seva base teòrica, s'enfronta a la reticència a posar valor monetari a la salut i es critica per valorar més altament les intervencions desitjades per aquells amb major riquesa. En l'àmbit sanitari, suposicions com la competència perfecta del mercat i la informació completa dels consumidors no solen ser vàlides, la qual cosa limita la seva aplicació.
Capítol 2: El Quality-Adjusted Life Year (QALY) El QALY es defineix com el valor d'una intervenció en salut, calculat multiplicant el canvi en el valor de l'estat de salut (en una escala de 0 a 1) pel canvi en els anys de supervivència. L'enfocament QALY és ambiciós, ja que busca comparar intervencions en totes les especialitats. La seva sensibilitat depèn del nombre d'estats de salut identificats.
Es discuteixen els criteris generals per a les mesures de qualitat de vida relacionada amb la salut (hrqol):
- Fiabilitat: Un instrument fiable ha de produir resultats similars en administracions repetides o per diferents observadors. La subjectivitat de la valoració dels estats de salut pot presentar problemes.
- Validesa: Un instrument és vàlid si mesura allò que pretén mesurar. Com que no hi ha un "estàndard d'or" per a la hrqol, es recorre a la "validació de constructe", que busca relacions sistemàtiques amb altres mesures.
El llibre aborda els problemes intrínsecs de l'enfocament QALY:
- Maximització de la Salut: L'objectiu de maximitzar la salut en termes de QALY implica que cada individu compta per igual, independentment dels seus ingressos. Això pot generar controvèrsia entre els metges, que prioritzen l'atenció individual.
- Equitat: L'enfocament QALY és igualitari, tractant la salut i cada any de vida per igual per a tots. No obstant això, se l'ha criticat per "ignorar la igualtat" (no tenir en compte la distribució preexistent de QALYs) i per ser "edatisme" (donar més importància a les intervencions en persones joves amb més anys de vida potencial).
- Valoració de l'Estat de Salut: Es qüestiona si els enquestats entenen adequadament la tasca de comparar estats de salut amb la mort. No obstant això, es considera un intent necessari per estructurar el problema de la priorització de l'atenció sanitària.
- Treball Empíric de Nord: Destaca que l'objectiu simple de "minimitzar el cost per QALY" entra en conflicte amb el "principi de rescat" (prioritzar els pitjors) i la idea que els igualment malalts tenen iguals drets a tractament.
Finalment, es descriuen els principals enfocaments per determinar els valors QALY:
- Escala de Puntuació (Rating Scale) i Estimació de Magnitud (Magnitude Estimation): Mètodes més senzills, encara que manquen d'una base teòrica explícita i la interpretació dels valors pot ser difícil. L'Estimació de Magnitud es va utilitzar en el desenvolupament del QALY de Rosser-Kind.
- Intercanvi de Temps (Time Trade-Off): L'individu valora quants anys de salut plena serien equivalents a un cert nombre d'anys en un estat de salut determinat.
- Intercanvi de Persones (Person Trade-Off): Es demana als enquestats que triïn entre curar un grup de 'n' persones en un estat de salut P o un nombre diferent de persones en un estat de salut Q. Aquest mètode s'acosta més a les decisions de política sanitària.
- Apuesta Estàndard (Standard Gamble): Basat en la teoria de la utilitat, implica que l'individu tria entre viure en un estat de salut H amb certesa o una aposta que pot resultar en salut plena o mort immediata. Tot i ser teòricament sòlid, pot ser difícil d'entendre pels enquestats i es centra en el valor individual, no social.
Capítol 3: Dues Mesures de QALY S'analitzen dues eines multi-atributs d'utilitat (MAUIs) destacades:
- EQ-5D (EuroQol): Desenvolupat per a la comparació de resultats basats en un conjunt comú de característiques de hrqol. Classifica els estats de salut en cinc dimensions amb tres nivells cadascuna, generant 245 estats. La valoració es va realitzar principalment mitjançant el mètode Time Trade-Off. S'ha demostrat la seva fiabilitat i validesa en diverses aplicacions. Una reserva és que els enquestats van avaluar els estats de salut independentment dels recursos assignats al seu tractament.
- Índex Rosser-Kind (R-K): L'exemple original d'enfocament directe per a QALYs. Es va desenvolupar a partir d'un projecte de mesura de resultats hospitalaris, identificant dues dimensions (discapacitat observada i patiment subjectiu) amb vuit i quatre nivells respectivament. Els estats de salut es van valorar utilitzant l'Estimació de Magnitud, emfatitzant la proporció de recursos que els jutges considerarien apropiada assignar a cada cas. Un aspecte únic va ser la resolució de contradiccions en les valoracions. Tot i que la mostra era petita, les seves valoracions han generat un gran interès. La seva fiabilitat es va demostrar amb una alta taxa d'acord en el test-retest. S'ha trobat validesa convergent amb el Nottingham Health Profile i el mètode Person Trade-Off. Malgrat algunes crítiques, el seu valor rau en l'èmfasi en les eleccions socials i la correcció d'inconsistències.
Capítol 4: Prova d'una Mesura de QALY Aquest capítol distingeix entre perfils de salut (escales ordinals sense punt de partida comú) i mesures QALY (escales cardinals amb un punt zero i un de salut plena comuns). La prova principal de les mesures QALY és la validació de constructe, comparant el rànquing d'estats de salut de pacients amb el que produeixen els perfils de salut. Es descriuen dos perfils de salut:
- Functional Limitations Profile (FLP): Versió del Regne Unit del Sickness Impact Profile (SIP), que mesura la hrqol en diverses dimensions (física, psicosocial, menjar i beure, comunicació, treball) i assigna un valor numèric per a la limitació funcional total.
- Nottingham Health Profile (NHP): Utilitza diverses dimensions separades, produint múltiples puntuacions en lloc d'una sola.
Els estudis de Whynes i Neilsen (1993) i McCulloch (1998) van comparar les dades de Rosser-Kind amb el NHP i el FLP, respectivament, demostrant una validació convergent significativa per a la mesura R-K. S'argumenta que, tot i que les correlacions no són perfectes, l'enfocament QALY és el més raonable per a la determinació de prioritats en salut, ja que encapsula la informació essencial sobre l'impacte en la salut.
Capítol 5: Comparació de Procediments Mitjançant Valors QALY Aquest capítol mostra com es poden utilitzar els valors QALY en anàlisis de cost-eficàcia per comparar intervencions, amb l'objectiu de maximitzar l'impacte sanitari amb un pressupost limitat. Es compara la cirurgia de bypass (CABG) i l'angioplàstia (PTCA) utilitzant dades Rosser-Kind i FLP. S'introdueix una tècnica gràfica per visualitzar la relació cost per QALY entre dos procediments i realitzar anàlisis de sensibilitat per avaluar com els canvis en costos o resultats QALY afecten les conclusions.
Capítol 6: Ús dels QALYs a la Pràctica S'analitzen els reptes pràctics de l'aplicació dels QALYs, basant-se en l'experiència del projecte de recerca de McCulloch (1998).
- Mesura i Responsabilitat: Les definicions de procediments poden canviar i la diagnosi pot ser subjectiva (ex: cirurgia cardíaca), generant incertesa en la recollida de dades i dificultant la predicció de resultats.
- Representativitat de la Mostra: La representativitat pot variar amb el temps degut a canvis en l'opinió clínica, la tecnologia i la definició de la "necessitat del pacient".
- Evidència d'Assaigs Clínics Aleatoritzats (RCT) per a l'Estimació de la Supervivència: Els RCTs tenen limitacions ètiques (no es pot negar un tractament establert a un grup de control) i metodològiques (les mostres són unrepresentatives, els resultats no són fàcilment generalitzables a la pràctica clínica real). Això posa en dubte la fiabilitat de les estimacions de supervivència dels metges per determinar el valor QALY.
Per abordar aquests problemes, el llibre proposa un enfocament alternatiu per a la gestió estratègica d'un sector sanitari, basat en l'Indicador de QALY Esperat Mitjà (MEQI):
- El MEQI es construeix recollint dades QALY i clíniques de cada pacient en un sector (ex: cardíac) a intervals regulars. Permet avaluar el rendiment d'un sector en termes d'impacte en la salut i costos al llarg del temps.
- El Dèficit de QALY Esperat (EQD) es proposa com a mesura de la "necessitat" d'un sector, calculat com la diferència entre el MEQI de la població general i el MEQI del sector, multiplicat pel nombre de pacients. L'EQD pot ser una base més objectiva per a l'assignació de recursos entre sectors, ja que es basa en anàlisis científiques en lloc de judicis mèdics individuals. S'assenten les bases per a una avaluació de la cost-eficàcia basada en el MEQI.
Capítol 7: El Cas de la Malaltia d'Alzheimer S'examina la dificultat de valorar la salut i prendre decisions en el context de la Malaltia d'Alzheimer (MA), donada la seva complexitat, la falta de cura, i els reptes per a la recollida de dades en RCTs.
- L'enfocament de les companyies farmacèutiques: Han justificat l'adopció de fàrmacs per a la MA (donepezil, rivastigmina) demostrant que redueixen els costos dels serveis de salut, basant-se en assajos clínics multinacionals i la relació inversa entre la puntuació de l'MMSE (Mini-Mental State Examination) i els costos d'atenció. No obstant això, es qüestiona la validesa de l'MMSE, la fiabilitat dels models a llarg termini i la valoració del temps de cuidadors informals.
- L'Assaig de Vigilància Post-Comercialització Estesa (EPMST): Es proposa com un mètode millor per a la MA que els RCTs, ja que es dissenya per estar el més a prop possible de la pràctica rutinària i descriure el sector de la malaltia en lloc de provar hipòtesis. L'EPMST podria proporcionar dades per a un PBMA i la implementació del MEQI en el sector de la demència, utilitzant la qualitat de vida del cuidador com a proxy per la del pacient.
- L'enfocament de la Retícula (Lattice Approach): Per a un nombre limitat de pacients, aquest mètode ofereix una manera de prendre decisions transparent sense requerir la mesura formal dels estats de salut o dels impactes econòmics, utilitzant descriptors binaris per preservar la complexitat de cada cas individual.
Capítol 8: L'Evidència ASTEC Aquest capítol examina l'estat actual de l'avaluació d'intervencions sanitàries (EHI) a Europa, segons el projecte ASTEC. L'EHI és més àmplia que la CEA o l'avaluació econòmica.
- El context: Les creixents expectatives, l'envelliment de la població i la pressió per obtenir valor pels diners han impulsat l'EHI. Els governs exigeixen cada cop més evidència de cost-eficàcia ("quart obstacle") per a l'aprovació de nous productes, especialment fàrmacs.
- Directrius Irlandeses Proposades: Es presenten com a exemple de directrius nacionals, que busquen assegurar que només s'adoptin les tecnologies que ofereixen "millor valor" en termes de resultat de salut per unitat de cost, requerint anàlisis econòmiques com CEA, CUA i CBA.
- Activitat EHI No Comercial a la UE: Hi ha una gran variació entre països en la quantitat i tipus d'EHI, amb la majoria centrada en la seguretat, eficàcia i efectivitat de productes individuals, i menys en l'eficàcia comparada o la cost-eficàcia. S'observa una manca general d'incentius i mecanismes per traduir l'evidència robusta a la pràctica.
- EHI Industrial: La indústria farmacèutica té el major pressupost per a EHI, que s'utilitza principalment durant el desenvolupament i llançament de nous fàrmacs. El "quart obstacle" ha influït en els assajos clínics, que ara mesuren resultats de qualitat de vida i costos. L'avaluació de dispositius mèdics és menys freqüent a causa de temps de desenvolupament més curts i menys preocupacions reguladores. Les fortaleses inclouen el rigor i la prevenció de desastres, mentre que les febleses són la curta durada dels assajos, la comparació freqüent amb placebo en lloc d'alternatives, i la manca d'evidència sobre l'ús rutinari.
- Desafiaments: La necessitat de major transparència i la creació de xarxes multi-disciplinàries i multi-nacionals per a l'intercanvi d'informació. Es reconeix que les comparacions de cost-eficàcia són cares i que l'eficàcia pot variar entre països.
Capítol 9: Revisió El llibre conclou que la valoració de la salut és una tasca ineludible i complexa, però necessària per millorar la presa de decisions en el sector sanitari. Reitera que, tot i els problemes de fiabilitat i validesa inherents a la mesura de la hrqol, les mesures QALY (com l'EuroQol) ofereixen la millor base per fer explícites les eleccions sanitàries. El MEQI i l'EQD es presenten com a eines prometedores per a l'anàlisi científica del rendiment del sector i l'assignació de recursos, respectivament, superant les limitacions del judici mèdic individual i els RCTs. La valoració de la salut a la pràctica és variable, i tot i la introducció de directrius, encara hi ha una manca de mecanismes fiables per difondre l'evidència científica.
En definitiva, McCulloch defensa que la valoració de la salut és factible i convincent, i que les mesures QALY són fonamentals per afrontar les futures crisis sanitàries.