Alternatives To The QALY For Comparative Effectiveness Research
Novel Approaches to Value Assessment Beyond the Cost-Effectiveness Framework
Des d'aquí he mostrat repetidament les dificultats de la fixació de llindars d'anys de vida ajustats per qualitat per decidir cobertura i copsar així el valor de la longevitat i qualitat de vida de les opcions terapèutiques. Avui recupero alguns materials recents que busquen anar més enllà d'aquesta mesura. Es tracta d'una orientació nordamericana perquè les lleis allà no afavoreixen la seva utilització, ans el contrari.
Poso tres referències, una al blog de Health Affairs, un altre oficial, i una tercera de ISPOR. Les alternatives tampoc són del tot satisfactòries però contribueixen al debat.
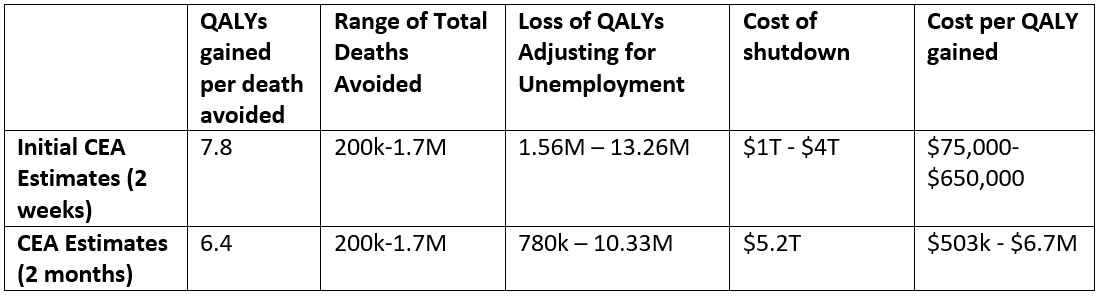
Ara que Medicare ha de fixar preus màxims per primera vegada, necessita un esquema i aquí va la comparació del que pot fer:
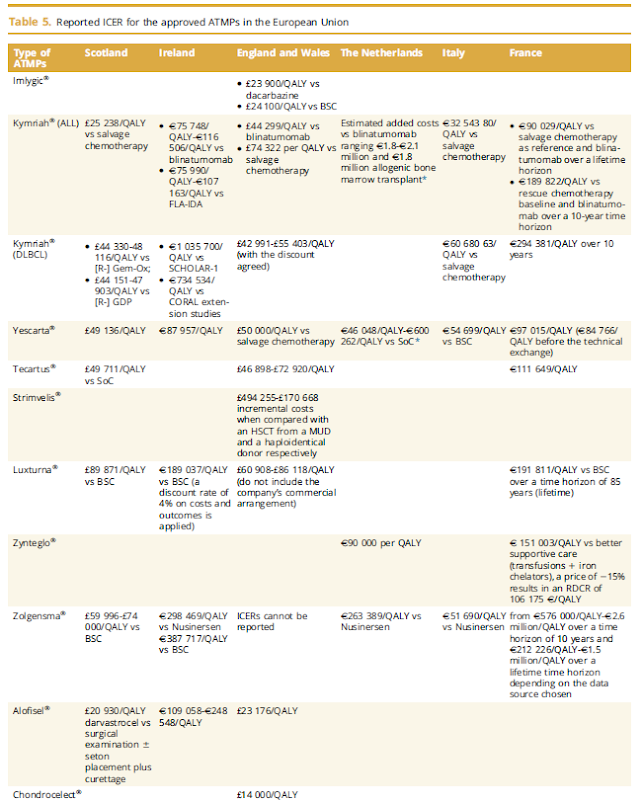
Illustrative comparison of different approaches for CMS to set a maximum fair priceSource: Illustrative evaluation based on author opinion. Notes: evLYG is equal value of life year gained. GRACE is generalized risk-adjusted cost-effectiveness. QALY is quality-adjusted life year. R&D is research and development. Low/Moderate/High refer to the potential of each criterion to achieve the objective.
Cost-effectiveness thresholds per quality-adjusted life-year (QALY) ranged between US$87 (Democratic Republic of the Congo) and $95 958 (USA) and were less than 0·5 gross domestic product (GDP) per capita in 96% of low-income countries, 76% of lower-middle-income countries, 31% of upper-middle-income countries, and 26% of high-income countries. Cost-effectiveness thresholds per QALY were less than 1 GDP per capita in 168 (97%) of the 174 countries. Cost-effectiveness thresholds per life-year ranged between $78 and $80 529 and between 0·12 and 1·24 GDP per capita, and were less than 1 GDP per capita in 171 (98%) countries.
Si voleu conèixer també les limitacions, s'expliquen a aquest comentari.