Redefining obesity: advancing care for better lives
Definition and diagnostic criteria of clinical obesity
El concepte d'obesitat ha estat objecte de controvèrsia tant en la seva definició com en la seva mesura. I per tant, quan significa un risc per a la salut i quan és una malaltia. Ara hi ha un nou informe que ajuda a situar les coses. Destaco un missatge:
Per començar, les dades epidemiològiques actuals sobre la prevalença de l'obesitat, que es basen únicament en l'IMC, s'han d'actualitzar amb noves mesures per reflectir l'obesitat real
Convé doncs refer les estadístiques quan més aviat millor. Altrament seguirem a les palpentes.
I aquí ve resumit l'editorial amb IA:
Aquest article editorial de The Lancet Diabetes & Endocrinology presenta la nova definició i el marc de diagnòstic de l'obesitat clínica publicats per la Comissió el 14 de gener de 2025. La Comissió busca canviar la manera com es pensa sobre l'obesitat, identificant quan és un factor de risc (obesitat preclínica) i quan representa una malaltia per si mateixa (obesitat clínica).
La Comissió, liderada pel Professor Francesco Rubino del Kings College London, va sorgir del reconeixement que, malgrat que l'obesitat afecta gairebé una vuitena part de la població mundial, no s'ha arribat a un consens global sobre la seva classificació i definició. L'article destaca que les persones amb obesitat tenen perfils de salut i necessitats diferents, però sovint es tracten com una única entitat definida per un sol paràmetre (l'IMC) o no es discuteixen en absolut. Les converses inicials entre els editors de la revista i Francesco Rubino fa 5 anys van portar a la formació d'aquesta comissió, un esforç de col·laboració que va incloure 56 experts de països d'ingressos alts, mitjans i baixos, representant una àmplia gamma d'expertesa. Aquesta col·laboració va implicar reunions regulars per compartir opinions i experiències per fer avançar la Comissió. La Comissió va ser anunciada formalment el març de 2022 i, en el moment de la publicació, ha estat avalada per més de 75 organitzacions mèdiques internacionals interessades en l'obesitat i l'atenció de les persones afectades.
La nova definició, basada en l'evidència, distingeix entre "obesitat clínica", una malaltia crònica i sistèmica causada directament per un excés d'adipositat, i "obesitat preclínica", una condició d'excés d'adipositat sense disfunció orgànica actual ni limitacions en les activitats diàries, però amb un major risc de salut futur. Donades les limitacions de l'IMC, la Comissió utilitza altres mesures de la mida corporal (circumferència de la cintura, relació cintura-maluc o relació cintura-altura), a més de l'IMC, per definir l'estat d'obesitat.
L'article subratlla que l'accés equitatiu a l'atenció continua sent un problema global important, per la qual cosa era vital que els canvis proposats per la Comissió poguessin utilitzar-se i aplicar-se en diversos entorns i ubicacions. L'IMC segueix sent la referència per la seva facilitat d'ús sense necessitat de recursos costosos, i per tant, les noves mesures de la mida corporal haurien de ser igualment fàcils de dur a terme. No obstant això, la necessitat d'una avaluació mèdica més profunda de l'obesitat podria augmentar la càrrega de treball i les pressions de temps sobre els professionals de la salut i, amb això, els costos. Malgrat això, continuar amb el marc de diagnòstic actualment imprecís podria generar una càrrega i uns costos encara majors, tant per als sistemes de salut com per a les persones amb obesitat.
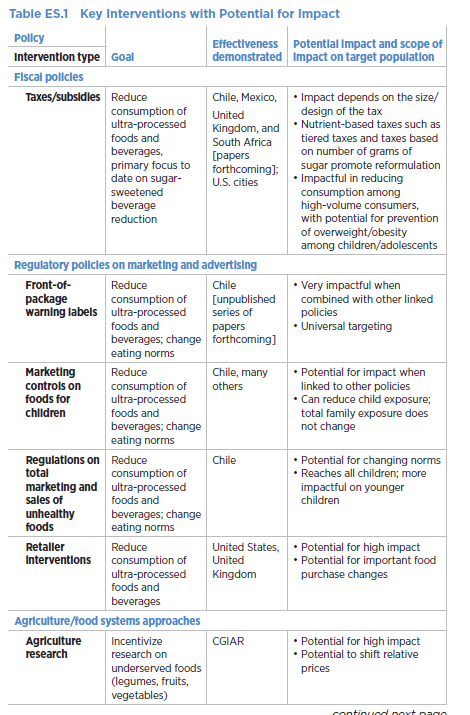
La implementació d'aquest nou marc de diagnòstic hauria d'obrir les portes a una gestió més accessible i eficaç de l'obesitat. Les polítiques existents per a l'accés a l'atenció (és a dir, cirurgia o medicació) són inadequades i s'haurien d'actualitzar per a una priorització rendible de les persones que més necessiten aquestes intervencions. Per a aquelles persones classificades amb obesitat preclínica, la mitigació del risc serà una prioritat clau. Les persones amb menys risc podrien gestionar-se principalment mitjançant canvis en l'estil de vida; no obstant això, cal més treball per identificar aquelles amb un risc augmentat que podrien requerir una intervenció mèdica.
L'article planteja com aquest replantejament de l'obesitat canvia el que sabem sobre la seva epidemiologia. Per començar, les dades epidemiològiques actuals sobre la prevalença de l'obesitat, que es basen únicament en l'IMC, s'han d'actualitzar per reflectir l'obesitat real. S'estan realitzant auditories preliminars de les bases de dades disponibles i suggereixen que un nombre substancial de persones amb obesitat no compleixen els criteris per a l'obesitat clínica. No obstant això, aquestes anàlisis estan limitades per l'ús de dades històriques i incompletes. Per tant, les bases de dades han d'incloure una imatge més completa de l'estat de salut individual. A més, hi ha un àmbit substancial per a l'estratificació de l'obesitat clínica en diferents subtipus, potencialment basats en la seva presentació clínica o fisiopatologia, cosa que hauria de permetre una millor gestió i comprensió.
En conclusió, l'article destaca que l'adopció d'un enfocament nou i més precís per a la identificació de l'obesitat i el canvi de les percepcions socials requeriran temps i esforç, però l'objectiu principal d'aquestes propostes és millorar la vida de les persones amb obesitat. Es presenta com una oportunitat per transformar l'atenció de l'obesitat, passant d'un sistema en què les persones es veuen sota una única etiqueta a un sistema que reconeix la salut i les necessitats úniques de cada persona.