The New Science of Aging Can Predict Your Future
Avui excepcionalment introdueixo un article d'Eric Topol al NYT traduït (per Google). Per guardar i reflexionar. El que està plantejant Topol és radical i modifica el plantejament de Geoffrey Rose, de dalt a baix. Ens caldrà llegir el seu nou llibre, Super Agers, que surt en tres setmanes, per copsar exactament el que proposa.
La nova ciència de l'envelliment pot predir el vostre futur
Opinió | Com viure més saludablement durant més temps - The New York Times
El somni de revertir l'envelliment ha captivat els humans durant segles, i avui la ciència està més a prop que mai d'assolir aquest objectiu. És a dir: encara està bastant lluny.
Això no és per falta d'intentar-ho. Alguns investigadors estan intentant reprogramar les cèl·lules per fer-les biològicament més joves, cosa que s'ha demostrat que inverteix les característiques de l'envelliment en animals més grans. Malauradament, això també pot provocar càncer. Altres investigadors estan estudiant fàrmacs anomenats senolítics, que tenen com a objectiu eliminar les cèl·lules envellides del cos. Tanmateix, també poden destruir altres cèl·lules que els humans necessiten per sobreviure.
Les transfusions de sang de ratolins joves semblen rejovenir els ratolins grans, però les empreses que ofereixen aquest tractament no provat per als humans estan cobrant molt per una teràpia potencialment perillosa. I tot i que alguns entusiastes de la longevitat prenen el fàrmac rapamicina perquè els estudis han demostrat que ajuda els animals a viure més temps, també debilita el sistema immunitari i nos'ha demostrat que funcioni en les persones.
Trobo que aquests esforços són intrigants i val la pena continuar. Però la majoria de la gent no només vol viure fins als 110 anys. Vol allargar el temps que viu lliure de malalties greus, un concepte conegut com a salut. Per això, l'enfocament més sensat és reduir la càrrega de tres grans malalties relacionades amb l'edat: el càncer, les malalties del cor i els trastorns neurodegeneratius, com la malaltia d'Alzheimer. Pot ser menys cridaner, però és més assolible que mai.
S'estima que almenys el 80% dels casos de malalties cardiovasculars, el 40% dels casos de càncer i el 45% dels casos d'Alzheimer es poden prevenir. Fins i tot amb un llarg retard (aquestes malalties poden trigar 20 anys o més a desenvolupar-se), els investigadors han lluitat per definir amb precisió el risc d'una persona amb prou antelació com per intervenir eficaçment. Per descomptat, algú pot fer-se una prova genètica i saber que té un risc més gran de patir la malaltia d'Alzheimer, però de què serveix això si no sap si la malaltia apareixerà aviat, als 95 o no?
En un futur proper, és possible que els metges no només puguin identificar si una persona té un alt risc de patir una malaltia greu relacionada amb l'edat; també poden predir quan és més probable que es manifesti aquesta malaltia i amb quina rapidesa podria progressar. Diversos descobriments recents de la ciència de l'envelliment fan que això sigui cada cop més possible.
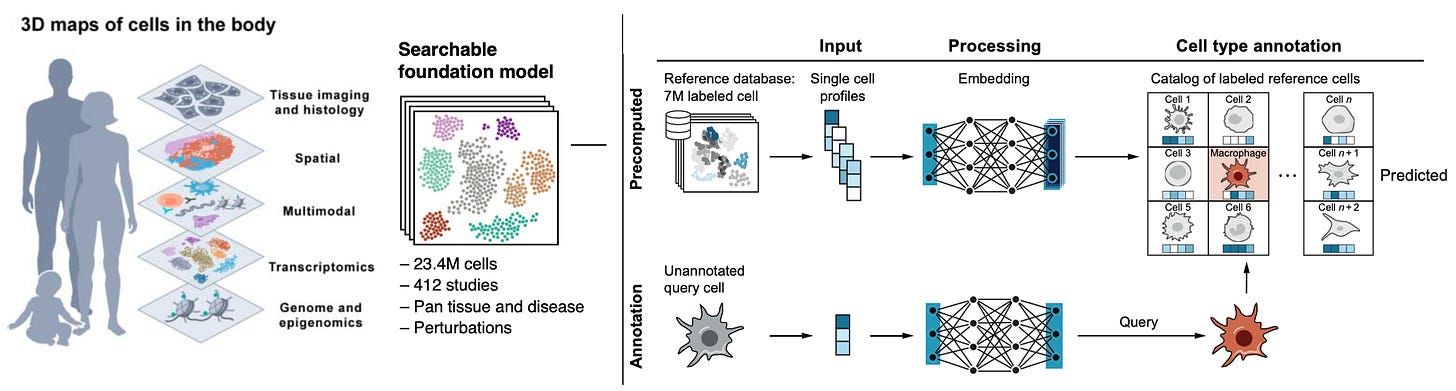
Des de la dècada de 2000, els científics han utilitzat la seqüència genètica d'una persona per calcular el seu risc heretat de certes malalties. En els últims cinc anys, la quantitat de dades que el camp mèdic pot recollir sobre la salut d'una persona ha augmentat. Més enllà de les eines tradicionals, com ara els registres mèdics, els resultats de laboratori de rutina i les imatges, els metges poden extreure una sèrie de rellotges biològics que ajuden a fer un seguiment de l'envelliment del cos.
Per exemple, els científics ara poden mesurar milers de proteïnes d'un sol vial de sang per generar el que s'anomenen rellotges d'òrgans proteòmics. Aquests rellotges descoberts recentment poden estimar el ritme d'envelliment del cervell, el cor, el fetge, els ronyons i el sistema immunitari. Aquests rellotges poden revelar, per exemple, si el cor d'una persona envelleix més ràpidament que la resta del seu cos, com un mecànic de cotxes que descobreix que tot funciona com hauria de ser, excepte els frens posteriors. Altres rellotges moleculars poden calcular l'edat biològica d'una persona en comparació amb la seva edat cronològica. El més estudiat és l'anomenat rellotge epigenètic, una lectura de parts del nostre ADN que es poden extreure d'una mostra de saliva. Les noves anàlisis de sang també poden detectar els primers signes de les tres principals malalties relacionades amb l'envelliment.
La superposició de tota aquesta informació biològica amb els avenços recents en intel·ligència artificial permet als proveïdors de salut fer prediccions cada cop més sofisticades sobre la probabilitat d'una persona de desenvolupar una malaltia.
Preneu una persona que vulgui determinar el seu risc de patir la malaltia d'Alzheimer. Ara es pot sotmetre a una anàlisi de sang per a una proteïna que quantifica l'acumulació de placa al cervell associada a la malaltia. Aviat, un metge també podria utilitzar un rellotge d'òrgans proteòmics per avaluar si el seu cervell sembla estar envellint més ràpid que la resta del seu cos o analitzar una foto de la seva retina, una eina emergent que, quan es combina amb la IA, pot ajudar a estimar la probabilitat de desenvolupar la malaltia d'Alzheimer en els propers cinc o set anys. Hi ha proves similars que es poden fer per avaluar el risc de càncer i malalties del cor.
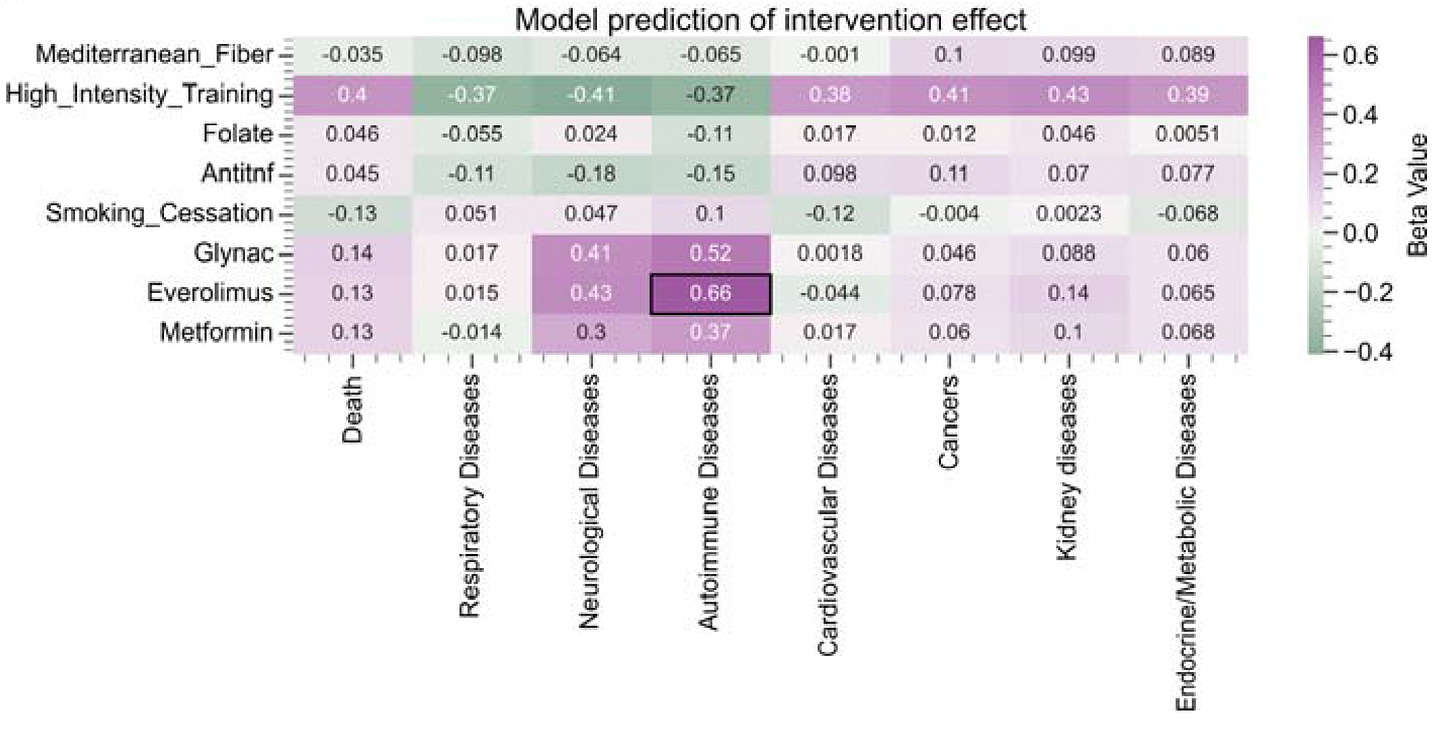
Aquest nivell de coneixement pot donar lloc a una nova manera d'abordar aquestes malalties: vigilància activa combinada amb canvis agressius d'estil de vida. Una persona considerada d'alt risc d'Alzheimer es pot sotmetre a avaluacions regulars i imatges cerebrals mentre pren mesures preventives per reduir el seu risc. Això podria incloure reduir els aliments ultraprocessats, augmentar l'activitat física i abordar qualsevol canvi en la pèrdua d'audició o visió, factors que poden influir en el declivi cognitiu. Els metges també podrien recomanar prioritzar el son, reduir l'alcohol i l'aïllament social o fer-se la vacuna contra el teules, que recentment s'ha demostrat que redueix el risc de demència. Alguns també podrien considerar prendre GLP-1, fàrmacs per a la diabetis i per perdre pes, que semblen reduir la inflamació nociva al cervell i al cos i que s'estan provant en assaigs clínics per prevenir l'Alzheimer.
Reunir aquesta informació mèdica i convertir-la en plans individuals per prevenir malalties cròniques és diferent de l'enfocament actual. Els protocols de detecció del càncer, per exemple, depenen en gran mesura de l'edat d'una persona. Aquí també és on els models d'IA poden beneficiar millor la medicina. Aquests models estan millorant en precisió i raonament i algun dia podrien incorporar dades dels nostres microbiomes intestinals o sistemes immunitaris per fer les prediccions de malalties encara més precises.
Fer-ho bé requerirà més estudi i inversió. No volem agreujar les desigualtats sanitàries fent que aquest tipus d'atenció mèdica només sigui accessible a uns pocs rics. Les reduccions importants de l'administració de Trump en el suport governamental a la investigació mèdica atenuaran aquestes perspectives.
Obtenir una injecció de sang juvenil o prendre l'últim suplement anti-envelliment de moda pot semblar una drecera per a una vida més llarga. Però allargar els anys que la gent viu sense la càrrega de les principals malalties relacionades amb l'edat és el que hauria de ser una prioritat nacional.
El Dr. Eric Topol és professor i vicepresident executiu de Scripps Research. És cardiòleg en exercici de la Clínica Scripps a La Jolla, Califòrnia. Aquest assaig està adaptat del seu proper llibre, "Super Agers: An Evidence-Based Approach to Longevity".
PS. Què cal fer per la prevenció de l'Alzheimer?