04 de setembre 2014
Dynamic risk adjustment in provider's payment
Adjusting Medicaid Managed Care Payments for Changes in Health Status
"Risk-adjustment methods have an inherent structural flaw that rewards preventable deterioration in enrollee health status and improved coding of disease burden", this is the key statement in Fuller et al. article. The answer they provide is the introduction of an additional payment adjustment according to changes in health status for similar mix of enrollees. The payment adjustment being proposed is based on changes in aggregate relative payment weights for all enrollees avoiding any individual adjustment.
This is a concrete application of the initial dynamic risk adjustment proposal that Eggleston et al. made in 2007. They suggested a two step payment system: a conventional risk adjustment (for variations in population health outside the provider’s control) and an additional one related to prevention efforts.
There is still a lot to learn about it. Let's keep an eye on this crucial topic.
PS. Have a look at Commonwealth Fund anouncement: "Our initiative recognizes that a wide range of factors influence providers’ choices, beyond financial rewards or penalties, including intrinsic motivation and medical professionalism, organizational influences, and policy" (see Box)
16 de juny 2020
Risk adjustment, a work in progress
This is a handbook on an unfinished topic. Risk adjustment is required for any managed competition model to work properly (Enthoven model) and for any funding of plans that tries to promote efficiency and avoid selection:
The Enthoven model has evolved as its ideas have been applied in particular institutional contexts. Today, sophisticated risk adjustment models give a regulator an effective tool to quantify differences among individuals in their expected healthcare costs. Rather than a system of risk-rated premiums, regulators rely more on risk adjustment to pay plans more for higher-risk enrollees. Also, the countries in which the regulated competition model has become dominant (e.g., Germany, the Netherlands) are characterized by separation of the functions of health insurance and healthcare provision. Regulated competition can and has been implemented without the presence of integrated HMO typeTherefore, any regulator interested in mitigating health insurance market failures should read it.
risk-bearing delivery systems. In these countries, and in other settings such as Medicare Advantage in the United States, regulated competition is oriented to the health insurers, not the healthcare delivery system.
Throughout this evolution, the key feature of Enthoven’s model remains: an active collective agent on the demand side of health insurance structures and manages the health plan market to overcome market failures. Enthoven calls this agent a “sponsor,” a role that can be fulfilled by various organizations. In health insurance markets today, sponsors are mainly governments (as is common in Europe and the United States) and employers (as is common in the United States). In this volume we will generally refer to a “regulator.”
31 de març 2021
Risk adjustment: a review
REINSURANCE, REPAYMENTS, AND RISK ADJUSTMENT IN INDIVIDUAL HEALTH INSURANCE
McGuire, Schillo and Van Cleef provide an additional perspective to conventional risk-adjustment. They say:
Reinsurance can complement risk adjustment of health plan payments to improve fit of payments to plan spending at the individual and group level. This paper proposes three improvements in health plan payment systems using reinsurance. First, we base reinsurance payments on spending not accounted for by the risk adjustment system, rather than just high spending. Second, we propose pairing reinsurance for individual-level losses with repayments for individual-level profits. Third, we optimize the weights on the risk adjustors taking account of the presence of reinsurance/repayment.
It sounds good, however technical requirements are demanding to be to implemented.
16 de desembre 2016
In search for the right approach to risk adjustment
Measuring risk-adjustment is crucial for avoiding risk selection incentives. Up to now, regression models have prevailed over categorical ones. However, such difference is often misunderstood or forgotten. A new article explains with all the details the comparison between both approaches.
The summary:
Regression and clinical categorical models represent very distinct approaches to risk adjustment. Users must carefully choose the model that best suites the intended application. Although clinical categorical models have many advantages in terms of communication, transparency, and stability, their initial development requires a significant effort and clinical input. Regression models usually require less initial development effort but are unstable in a changing environment and fail to provide the same degree of communication value and transparencyGreat work by Fuller et al. Though I fully support the categorical approach, my impression is that beyond such options, there are also alternatives that may fit better with morbidity data: mixed models (grade of membership). The following book explains the details (chap 17).
06 de desembre 2010
Referència clau
Quan algú es planteja compensar capitativament a una població ja sap que ha d'ajustar pel risc d'emmalaltir que tingui. El problema és quin és el cost legítim i aleshores la mitjana del cost poblacional es premia com a referència. Sabem que aquest opció és errònia i que penalitza els comportaments més eficients (efecte ratchett i regression to the mean amb el pas del temps). Al JHE podeu trobar l'article que proposa un esquema suggerent i aplicable per a resoldre un sistema de pagament capitatiu. Una referència clau a tenir en compte.
El resum:
A new method is proposed to assess and improve the performance of risk qualization models in competitive markets for individual health insurance, where compensation is intended for variation in observed expenditures due to so-called S(ubsidy)-type risk factors but not for variation due to other, so-called N(onsubsidy)- type risk factors. Given the availability of a rich subsample of individuals for which normative expenditures, YNORM, can be accurately determined, we make two contributions: (a) any risk equalization scheme applied to the entire population, YREF, should be evaluated through its performance in the subsample, by comparing YREF with YNORM (not by comparing YREF with observed expenditures, Y, in the entire population, as commonly done); (b) conventional risk equalization schemes can be improved by the subsample regression of YNORM, rather than Y, on the risk adjusters that are observable in the entire population. This new method is illustrated by an application to the 2004 Dutch risk equalization model
PS. Aquesta altra referència sobre el mateix tema al JHE no m'ha convençut "Capping risk adjustment?" i aquesta no gaire "Risk adjustment in health insurance and its long-term effectiveness". Ho rellegiré a veure si li sé trobar el què.
Trobareu alguns altres papers a Risk Adjustment Network
02 de juliol 2019
Episode groupers: a crucial tool for population health management
Summary of analytic components in selected episode groupers.
| Product | Episode example | Sample conceptual focusa | Number of episodes | Clinical setting | Public episode definition | Linked risk-adjustment approach |
|---|---|---|---|---|---|---|
| 3M Patient-focused Episode Software | Not reported. | • Event-based episodes per patient • Cohort-based episodes among patients with a shared condition or characteristic | >500 | All | No | 3M Clinical Risk Groups |
| Cave Grouper | Urinary tract infection | • Physician relative efficiency and effectiveness scores • High-cost patient prediction | >500 | All | No | CCGroup MediScreen |
| CMS-BPCI | Urinary tract infection | Inpatient and post-acute care | ~50 | Inpatient, skilled nursing facility, inpatient rehabilitation facility, long-term care hospital or home health agency | Yes | No |
| McKinsey & Company | Perinatal | Principal Accountable Provider | >100 | All | Yes | Yesb |
| Optum Symmetry Episode Treatment Groups | Pregnancy, with delivery | • Patient total cost of care by condition categories • Provider profiling | >500 | All | Yes | Optum Symmetry Episode Risk Groups |
| OptumInsight Symmetry Procedure Episode Groups | Radical hysterectomy | • Medical and surgical procedure cost • Provider profiling | ~200 | All | No | Optum Symmetry Episode Risk Groups |
| Prometheus Analytics | Pregnancy | Potentially avoidable complications | ~100 | All | Yes | Prometheus Analytics risk adjustment |
| Medical Episode Grouper | Cardiac arrhythmias | • Population profiling • Provider profiling | >500 | All | No | Disease Staging and Diagnostic Cost Groups |
13 de setembre 2020
Improving risk adjustment with reinsurance
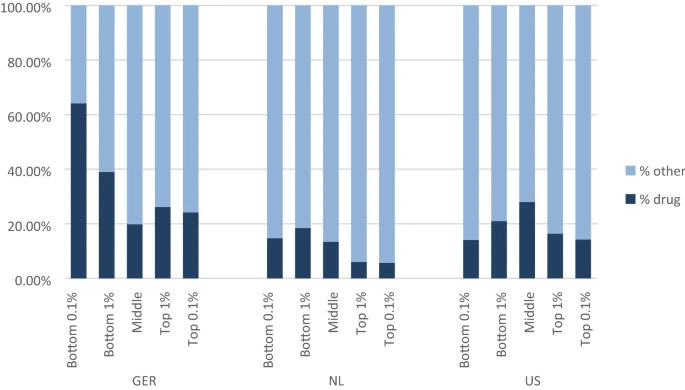
The high degree of persistence in membership in the extremes of the residual spending distribution in all three countries raises concerns that insurers might take steps to deter those who tend to be underpaid and attract those who tend to be overpaid. Attracting the healthy/deterring the sick among subsets of the populations with the disease indicators (such as diabetes) prevalent on both extremes of the residual spending distribution could be a highly profitable strategy, and potentially lead to distortions in the efficient care for these groups. In response to these findings, we proposed a form of reinsurance, based on residuals, and targeted to members of a “risk pool” defined on past-year very high undercompensation. Careful targeting (along with re-estimating the beta weights in risk adjustment to take into account the reinsurance payments) leads to very substantial improvements in overall fit of payments to spending, with especially large effects for the most extremely under- and overcompensated. The share of people affected by this form of risk sharing is very small, less than 3 in 1000 in all three countries. While our proposed policy seems effective in better tying payments to spending, there are alternative approaches to the same issue. One example would be to find ways to split groups like those with diabetes and other illnesses prevalent among the undercompensated into those likely to be on one or the other side of the residual spending distribution. Calling attention to the powerful effects members of the tails of the residual distribution have on the overall fit of the models is the first step in directing policy attention to these important groups.
08 de novembre 2023
Toca canviar l'actual sistema de pagament tronat
Guiding Risk Adjustment Models Toward Machine Learning Methods
Comparing risk adjustment estimation methods under data availability constraints
En aquells entorns on el mercat i el sistema de preus no hi juguen un paper, és on cal pensar en mecanismes alternatius per a crear incentius a l'eficiència i a la presa de decisions. El mecanisme de preus es altament poderós i ja ho deia Hayek és un senyal que permet coordinar les decisions.
Al sector salut no tenim preus competitius de mercat. Tenim en alguns casos tarifes, i habitualment el que en diem sistemes de pagament i d'ajust de risc. Ja fa dues dècades que ho va explicar Newhouse en aquest llibre. Hi ha tarifes perquè hi ha asseguradores amb poder de negociació que les imposen, o donen poc marge per modificar-les. No podem parlar de formació de preus competitius de mercat ni de bon tros. I hi ha sistemes de pagament allà on no arriba bé la definició de l'output o interessen altres objectius. Això succeeix tant en asseguradores privades com públiques.
Es clar, si pagues una tarifa per acte, incentives que es facin més actes. I el que interessa són els resultats de salut, no l'activitat en si mateixa. Aquí és on entren els sistemes de pagament.
Tinc la ferma impressió que aquesta qüestió no es pren amb el rigor que es mereix. Newhouse ja hi feia èmfasi fa molt de temps. Deia, si millorem el sistema de pagament, estarem millorant també l'eficiència del sistema de salut.
Atenent a la moda del moment, ara ens caldria també analitzar les noves eines d'ajust de risc basades en aprenentatge automàtic, si realment aporten millores o només són un miratge marginal. És a dir si aporten alguna cosa, a canvi d'oferir una caixa negra que no sabem com els factors contribueixen al resultat. La meva impressió per ara, és de caixa negra. Caldrà veure què va sorgint. Dels dos articles ressenyats al principi, el primer hi confia, mentre que el segon ja ho diu:
"Our findings show that ML techniques, particularly SL, outperformed OLS in all data scenarios, although the adjusted-R 2 RE ranges between 0.02% points in the coarse granularity/poor range of variables scenario and 2.8% points in the coarse granularity/rich range of variables scenarios, indicating no statistically significant gain in our sample of 100,000 observations. Performance based on MSE also showed consistent results"
Si del que es tracta és augmentar 2,8 punts percentuals la variació explicada, a canvi d'una caixa negra, ja us puc dir que no paga la pena. Deixem de banda l'aprenentatge automàtic per ara. Tornem allà on érem, als orígens. Fem un bon diagnòstic i corregim el que no funciona (que és molt).
A Catalunya, la situació dels sistemes de pagament requereix una profunda revisió que s'ha anat ajornant sistemàticament. Hi ha dos nivells, l'assignació poblacional (ajust de risc, pròpiament dit) i la compensació als proveïdors (sistema de pagament, pròpiament dit). No tenim ni l'un ni l'altre que facin la funció que hem dit que ha de fer, promoure l'eficiència i millorar la coordinació de les decisions. Podem seguir així? La regulació vigent aviat farà una dècada, és de 2014. Algú hauria de situar la seva revisió en profunditat com a prioritat. Està tronat.
PS. tronat -ada. 1 adj. [LC] Fet malbé per l'ús
PS. Disbarat del dia. Com la indústria farmacèutica posa dos preus diferents al mateix medicament, explicat a WSJ.
09 de març 2016
The building blocks of healthcare payment systems
The implementation of healthcare payment systems is a complex task for any insurer, either public or private. Any option for reform is path-dependant and uncertain. The context and the inertia are the sources of lack of support for a change, unless a larger amount of Money -a big carrot- is put on the table.
A new report highlights the building blocks of a payment system. This is the instruction manual, and it refers to 4 issues:
Building Block 1: Services Covered by a Single PaymentA must read, keep it for your files.
Option 1–A: Adding new service–based fees or increasing existing fees.
Option 1–B: Creating a treatment–based bundled payment for a single provider
Option 1–C: Creating a multi–provider treatment–based bundle.
Option 1–D: Creating a condition–based payment.
Option 1–E: Creating a population–based payment.
Building Block 2: Mechanism for Controlling Utilization and Spending
Option 2–A: Adjustments in payment (pay for performance)based on utilization.
Option 2–B: Adjustments in payment (pay for performance)based on spending or savings.
Option 2–C: Bundled payment.
Building Block 3: Mechanism for Assuring Adequate Quality and Outcomes
Option 3–A: Establishing minimum performance standards.
Option 3–B: Payment adjustments (pay for performance) based on quality.
Option 3–C: Warrantied payment
Building Block 4: Mechanisms for Assuring Adequacy of Payment
Option 4–A: Risk adjustment or risk stratification.
Option 4–B: Outlier payments.
Option 4–C: Risk corridors.
Option 4–D: Volume–based adjustments to payment.
Option 4–E: Setting and periodically updating payment amounts to match costs.
06 de març 2012
ROM
Més enllà d'un líquid espirituós caribeny de gamma extra, ROM és també l'acrònim de risc de mortalitat que avui és objecte de la meva atenció. Molt sovint veiem que s'utilitza la casuística per a comparar els resultats entre hospitals. A molts gerents els encanta veure's al podi dels millors, i aquells que no hi són aleshores es queixen de l'eina de mesura. Hem de convenir que la tecnologia que es relaciona amb la mesura de la casuística hospitalària està desfasada en el temps. Destaco els dos problemes principals, (1) les activitats ambulatòries dins l'hospital i els costos que representen queden desdibuixats en la mesura de la causística per DRGs actual i (2) l'índex de casuística, el mecanisme d'agregació ordinal mitjançant pesos relatius provoca unes pèrdues d'informació extraordinàries que el fan en moltes ocasions incomprensible i poc acurat per ajustar les malalties tractades a un hospital i comparar-les amb l'estàndar. Des de fa anys s'ha intentat avançar en versions de DRG que incorporessin gravetat, i d'aquesta forma tenim els APR-DRG.
Ara bé, en Norbert Goldfield també fa més temps encara, va pensar que la incorporació de dades clíniques a la mesura de la casuística podria modular amb més precisió el que entenem per gravetat de veritat, la més greu de totes, el risc de mortalitat. I d'aquesta manera va considerar que les dades de laboratori podien permetre aproximar aquesta informació predictiva. I així ho va fer, i ara fa poc ho han publicat i malgrat que el resultat és força limitat, és una línia a tenir en compte.
PS. Ara com ara l'estimació de l'ajust risc de mortalitat per hospital als USA es fa des d'una altra perspectiva sobre la que hi ha un consens.
PS. La reformulació de l'ICS. El document que confirma l'obsolescència organitzativa.
PS. Lectura obligada: Victor Fuchs a NYT i el que pensa sobre la sanitat als USA:
Then what is the big thing we should do to change the system?The big thing for me is a dedicated value-added tax. It would provide universal coverage, a basic health care system for everyone. But the tax could be used only to pay for basic medical care, and basic medical care could be paid for only with the tax.We want to subsidize the poor and the sick. The value-added tax is a function of income — the poor and the sick would pay much less. People are free to buy more health insurance, but they would do it with after-tax dollars.We would do away with Goldman Sachs executives getting a $40,000-a-year health care plan that is tax-free. Patients would be enrolled in accountable care organizations, like the Kaiser plans in California. The plan gets a risk-adjusted capitation payment for each person enrolled.
12 d’agost 2019
14 de juny 2020
Measuring morbidity vs. measuring episodes: Two parallel views
In order to assess the health risk of a population there are two main options: Morbidity adjustment and Episodes of care. The first one can use Clinical Risk Groups, while the latter Patient focused episodes. The morbidity adjustment is useful for adjusting at population level, it is a categorical system, while episode measurement adjusts at patient level .
In this article you'll find an interesting application to a primary care center.
CRGs have definite value with respect to predicting health care utilization, but it is important to note the limitations of the CRG as a stand-alone classification of complexity, particularly for the categorization of patients in the health status 1 throughThe article is trying to use the CRGs for episode measurement, and this is a wrong approach. CRGs are useful as a whole picture, physicians need details, only episodes can provide such information.
5 categories. In order to enhance the accuracy, relevance and predictive value of the CRG classification methodology, we see great value in pursuing methods that allow for the careful and systematic inclusion of information from the care record.
05 de juliol 2019
Far away from blackbox medicine
BIG DATA I REAL WORLD DATA EN L'ANÀLISI DE LA UTILIZACIÓ, SEGURETAT I EFECTIVITAT DE MEDICAMENTS, TECNOLOGIES I INTERVENCIONS SANITÀRIES
The main speech of a next workshop is about causal inference by Miguel Hernan. If you want to have a look at his book, you'll find it here.
Causal inference is one of the main issues that current machine learning methodologies often try to skip. Finally we do need to know the factors, the causes that produce a consequence, a disease. And for example with risk adjustment, it happens the same. The methodology has to provide a clear understanding of the factors for adjustment and weights. Otherwise it would be a blackbox.
13 de juliol 2023
Una nova mesura de la morbiditat poblacional
En Randy Ellis ja abans de la pandèmia estava apuntant cap un nou sistema que permetés la mesura de la morbiditat amb dades diagnòstiques sense una classificació categòrica dels pacients. És a dir es tracta d'una evolució dels models que ell ha proposat des de fa anys junt amb Arlene Ash, els DCGs, i alhora una evolució del Clinical Classification Software.
L'objectiu:
Our objective was to create a clinically detailed, transparent, well-documented, nonproprietary classification system suitable for predicting diverse outcomes using ICD-10-CM diagnostic information and share a core set of predictive models that can be used on other data sets and populations.
Els tres tipus:
We created 3 types of DXIs. The primary or main effect DXIs, called DXI_1, focus on clinical dimensions in each diagnosis. Diagnoses were assigned up to 4 DXI_1s. In some cases, we created both broader and narrower DXI_1s that overlapped because we did not know a priori the level of detail preferred for prediction. We illustrate this approach below in our discussion of sepsis and hypertension in pregnancy DXI_1s.
The second group, DXI_2 modifiers, cut across DXI_1s. Some identify disease severity, such as “with complications,” “hemorrhage,” “secondary,” “bilateral,” and “with coma.” Others may be useful for disease monitoring, including flags for future research and epidemiological surveillance, such as sexually transmitted and vaccine-preventable infectious diseases. Certain diagnoses for external causes and factors influencing health status (whose codes begin with V-Z) were not assigned a DXI_1 and were instead only assigned DXI_2 modifiers.
Finally, DXI_3 scaled variables capture test results, disease severity, or clinically relevant distinctions not easily captured in binary DXI_1 categories. These include body mass index (BMI; calculated as weight in kilograms divided by height in meters squared), neonatal birth weight, neonatal gestational age, pregnancy trimester, low vision/blindness stages, coma scale measures, stroke scores, and duration of unconsciousness. As an example, the DXI_3 variable for BMI, calculated as weight in kilograms divided by height in meters squared, takes on values between 18.5 and 70, corresponding to ordered groups of BMI ranges. When comparing the DXI classification system to existing models, we included only main effects (DXI_1s) as predictors. This comparison cleanly demonstrates the value of the DXIs richer classification of diagnoses. Quantifying the additional value of using DXI_2 and DXI_3 items is left for future research.
Exemples:
La capacitat predictiva en despesa, aquí:
Si això és així, caldrà provar-ho ben aviat, amb 2929 variables explicatives assoleix una variació explicada del 51%.
El software per provar-lo en SAS aquí.
14 d’abril 2021
Pandonomics
26 de juliol 2012
Persones malaltes, poblacions malaltes
Quan Geofrey Rose va escriure el seu article fonamental en epidemiologia - Sick individuals and sick populations - en realitat estava destriant quin ha de ser el fonament de les polítiques de la salut pública i les paradoxes que l'envolten. Al resum deia que l'origen de les malalties s'enfronta a dues qüestions, els determinants dels casos individuals, i els determinants de la taxa d'incidència:
If exposure to a necessary agent is homogeneous within a population, then case/control and cohort methods will fail to detect it: they will only identify markers of susceptibility. The corresponding strategies in control are the 'high-risk' approach, which seeks to protect susceptible individuals, and the population approach, which seeks to control the causes of incidence. The two approaches are not usually in competition, but the prior concern should always be to discover and control the causes of incidence.Això que s'escrivia el 1985 segueix sent d'interès, malgrat els necessaris matisos fruit de l'evolució del coneixement. Tot mirant l'informe sobre la salut dels catalans, veig que el 60% de les causes de la mortalitat evitable són susceptibles d'actuació mitjançant polítiques sanitàries intersectorials, mentre que el 40% seria per part dels serveis de salut. Caldria pensar doncs en l'estratègia poblacional de Rose en primer lloc si volem reduir més la mortalitat evitable que representa el 13,6% de les defuncions (16,2 H, 9,8 D). Hem d'estar satisfets que hagi disminuït un 14% entre 2005 i 2009, però cal restar amatents (p.105). Aquesta dada també incorpora una reducció de mortalitat per accidents de trànsit, 40% en cinc anys, i en certa mesura caldria ajustar-la per l'exposició al risc, que previsiblement ha disminuït amb la crisi.
Si voleu fer una ullada a les tendències de l'esperança de vida a Europa, mireu al IJE. Curiosament a l'informe que comento no es mostren aquest tipus de dades. S'en deuen haver oblidat.
PS. Reprodueixo el manifest del col·lectiu EMMA i m'hi adhereixo
What's really going on in Catalonia (Notes on the present financial crisis in Spain and the political options for Catalans)
A full-fledged bailout of Spain is now taken for granted by most observers. In the meantime, Mr. Rajoy's government has grudgingly agreed to submit its finances to external oversight and to implement some overdue reforms. It is unlikely, however, that the measures it has taken can actually put the country's economy on the right track. So far, they seem to be designed to raise money for the state's operation rather than to stimulate growth and create jobs. And while the need for austerity is unquestionable, there are serious doubts about the focus of the spending cuts and about the selective way in which they are applied. In fact, the central government is passing much of the pain on to the regional and local administrations, which are responsible for the provision of most basic services. We are already witnessing the damaging effect of those policies on the lives of citizens and some foreseeable angry reactions.
At first glance, and given the regions' histories of carefree spending while times were good, efforts to rein them in might seem reasonable. We shouldn't forget, however, that the central government itself has been just as guilty of wastefulness and poor management, and that it's still refusing to give up some very expensive and very questionable programs. Also, restrictions are imposed across the board, making no distinction between the communities that rely on their own money to pay for the services they provide and those that are essentially living –quite regally in some cases– on public funds that the central government has extracted from the former. And no regard is given to whether or not individual regional administrations have been acting to control their budgets and to put their house in order, or to how well they're doing on that count.
Admittedly, Catalonia's record in the making of today's crisis is not brilliant. Like other southern European societies, it got used to living beyond its means. The real estate boom, encouraged by cheap credit and slack financial and political supervision, created the illusion of riches that is at the root of the present troubles. At the same time, the irresponsible policies of previous regional administrations have left a poisonous legacy of public debt. Catalans have brought upon themselves much of their hardship, but their economy remains strong enough to overcome the situation, and their burden of public and private debt would be manageable in the short to medium term if Catalonia had full use of the revenue it generates.
But today we are facing a grotesque situation in which the central government –a net recipient of Catalan resources– threatens with intervention a community that was the first to implement painful austerity measures and whose economy, if given a chance to develop, could best ensure the state's economic viability. Indeed, long before Mr. Rajoy was finally compelled to act by the country's EU overseers, the Catalan administration under President Artur Mas had set out implementing an unpopular policy of fiscal adjustment. Now it is being asked by the central government to inflict on its citizens one more round of cuts that jeopardize not only the provision of services but also most productive investments in infrastructures, education or research that are essential for any society's future. In fact, the central government is demanding of Catalonia sacrifices that it wouldn't dream of imposing on itself.
***
Mr. Mas now finds his government's every move constrained by the dire need of financing for its day-to-day operation, while the necessary funds can be released or withheld by the central government essentially at its discretion. So far he has chosen to treat this as a strictly financial problem and, following this line, he's trying to reach with the other political parties in Catalonia a consensus position that could be a basis to renegotiate the fiscal relationship between Catalonia and the Spanish central government. However, some Catalan officials will admit in private that, even if that consensus could be found at home, the chances of an agreement with Madrid are almost nil. As long as the continuity of the Spanish project depends on the funds obtained from Catalonia, the central government can hardly afford to give Catalans a just financial deal without endangering the very survival of the state.
The ruling coalition would like to keep all its options open, but as things now stand Mr. Mas may well be running out of them. Essentially, he can insist on a negotiation and try to wring from the Spanish government some sort of compromise, even if he's aware that all he can expect is just another bad deal that would only postpone the inevitable showdown. Or he could go for a clean break with a state that doesn't feel it needs to sit and talk with a province that it can control absolutely as long as it holds the purse strings.
On the home front, influential players in the economic scene are reluctant to go along with any steps that could lead to a major confrontation with Spain. This is also the position taken by representatives of unionist parties in Catalonia, who insist on preserving the status quo even if it's clearly damaging for their constituents. No wonder this approach has made them lose support in every election.
On the other hand, a clean break is exactly what a large body of Catalans –civil society organizations, local councils, the rank-and-file of various parties and a growing number of private individuals– appears to be demanding from its leaders. The latest polls show support for independence at over fifty per cent, while the numbers of those squarely opposing it –now around twenty-one percent– continue to fall.
Understandably, economic grievances are cited by many of the Catalans who have been warming up to the idea of independence in the past few months. When citizens are being subjected to service cuts and tax hikes while a big chunk of the revenue they generate continues to be siphoned off by the central government, the economy would be a good enough reason for Catalans to give some serious thought to political separation from a state that is clearly working against their interests.
But it would be wrong to characterize this as a mere financial dispute between a province and its capital. There is a more fundamental disagreement, which is of a political nature and whose solution would imply a complete redefinition of the state that no one outside of Catalonia is even ready to consider. These deeper problems will be impossible to solve as long as Spain refuses to acknowledge the existence within the state of very diverse societies with conflicting sets of values and to revise some tenets that it regards as essential to its national being.
***
For a growing number of Catalans, Spain is a dead-end road, incapable of healing itself and offering them no perspectives except more of the same old systematic plunder of their hard-earned resources at the same time that it uses every opportunity to stamp out their national character. And they see the only way out in a peaceful, orderly and responsible process of political independence.
There are justified concerns, domestically and internationally, over the can of worms that a process of independence could open. Independence can indeed be messy, and today Europe and the world may think that they can ill afford an open conflict and an added source of instability. And yet, conflict is what has defined the relation between Catalonia and Spain for at least three hundred years, and instability –a systemic, unsolvable form of instability– is what we already have there. Conversely, the emergence of Catalonia as a solid political reality, creditworthy and ready to face up to its international obligations, would surely become a source of stability in the south of Europe.
As a result of the financial crisis, many outside observers have become aware of Spain's economic and political shortcomings, and some may now begin to see Catalonia as what it is –a viable and active community that is being made to pay for the incurable flaws of a political project that for three hundred years has been incapable of building a cohesive project for its constituent peoples.
Beyond their immediate difficulties, Catalans are now calling for a brand new long-term political project allowing the survival of an economic, social and cultural model that, in spite of all the obstacles and shortcomings, both external and self-imposed, has succeeded in building a relatively prosperous, creative and inclusive society.
In Catalonia today the people are well ahead of their government. They expect from their leadership that it takes on its responsibilities towards the present and future generations. If their government chooses to heed this call and throw its weight behind them, many more will come round. If it doesn't, Catalans are likely to forge ahead no matter what, either by their government's side or marching in front of it to show the only way to a better future.
These notes were prepared by Col·lectiu Emma and have the endorsement of a number of respected civil society representatives.
Alícia Adserà (Princeton University), Sebastià Alzamora (writer), Carles Boix (Princeton University), David Boronat (entrepreneur), Enric Bou (Università Ca' Foscari Venezia), Jaume Cabré (writer), Miquel Calçada (journalist and businessman), Salvador Cardús (Universitat Autònoma de Barcelona), Ramon Carner (Cercle Català de Negocis), Muriel Casals (Universitat Autònoma de Barcelona), Àngel Castiñeira (ESADE), Liz Castro (writer), Jordi Comas (architect), Xavier Cuadras (Universitat Pompeu Fabra), Jordi Cuixart (businessman), Ramon Folch (businessman), Jordi Galí (Universitat Pompeu Fabra), M Dolors Genovés (journalist and historian), Josep Ginebra (Universitat Politècnica de Catalunya), Modest Guinjoan (Universitat Pompeu Fabra), Jaume López (Universitat Pompeu Fabra), Josep Maria Lozano (ESADE), Isidor Marí (Universitat Oberta de Catalunya), Isabel-Helena Martí (businesswoman), Rita Marzoa (journalist), Francesc Mortés (businessman), Ferran Requejo (Universitat Pompeu Fabra), Joan Ramon Resina (Stanford University), Xavier Roig (writer and engineer), Jaume Soler (accoustician), Miquel Strubell (Universitat Oberta de Catalunya), Àlex Susanna (writer), Quim Torra (editor), Jordi Torras (entrepreneur), Matthew Tree (writer), Ramon Tremosa (MEP, Universitat de Barcelona), Jaume Vallcorba (Fundació Catalunya Estat), Jaume Ventura (Universitat Pompeu Fabra).
Endorsement's update: Update: Germà Bel (Universitat de Barcelona), Martí Boada (Universitat Autònoma de Barcelona), Susan Digiacomo (Universitat Rovira i Virgili), Josep Gifreu (Universitat Pompeu Fabra), Josep Maria Figueres (Universitat Autònoma de Barcelona), Jordi Graupera (journalist), Antoni Maria Piqué (journalist)
19 de febrer 2018
Public funding of succesful Pharma R&D
If we consider the 210 new molecular entities (NMEs) approved by the Food and Drug Administration from 2010–2016, then you'll find that NIH funding contributed to published research associated with every one. A PNAS article explains that:
Collectively, this research involved 200,000 years of grant funding totaling more than $100 billion. The analysis shows that 90% of this funding represents basic research related to the biological targets for drug action rather than the drugs themselves. The role of NIH funding thus complements industry research and development, which focuses predominantly on applied research. This work underscores the breath and significanceThis public funding is forgotten in the costs of a new molecule. Although in the price, the manufacturer surplus doesn't remunerate such contribution. Some adjustment should be applied, to be fair.
of public investment in the development of new therapeutics and the risk that reduced research funding would slow the pipeline for treating morbid disease.