Lessons for the United States from Pharmaceutical Regulation Abroad
Resumit amb IA
Aquí teniu un resum detallat de l'article "Lessons for the United States from Pharmaceutical Regulation Abroad", basat en els fragments proporcionats:
L'article analitza l'economia de les regulacions farmacèutiques, centrant-se en les lliçons que els Estats Units poden aprendre d'altres països d'ingressos alts. Comença assenyalant que els preus dels medicaments als EUA, especialment els de productes amb patents, són significativament més alts que en països com França, Alemanya, Japó o el Regne Unit. Aquesta disparitat de preus alimenta el debat sobre la necessitat d'intervenció governamental als EUA.
Per què cal la intervenció governamental en els mercats farmacèutics? L'article argumenta que els mercats farmacèutics no operen sota les condicions d'un mercat competitiu ideal a causa de diverses particularitats:
- Béns de credibilitat ("Credence Goods"): És difícil per als consumidors avaluar la qualitat i els efectes dels medicaments abans i fins i tot després de consumir-los. La regulació d'entrada per part d'agències com la FDA (als EUA) o l'EMA (a Europa) busca reduir aquesta asimetria d'informació, assegurant la seguretat i l'eficàcia, però al mateix temps, significa que no hi ha lliure entrada al mercat.
- Alts costos de desenvolupament i facilitat d'imitació: El desenvolupament d'un nou fàrmac és molt car. No obstant això, un cop establerta la seva seguretat i eficàcia, la imitació és relativament fàcil. Les patents i altres formes d'exclusivitat regulatòria protegeixen els innovadors, que d'altra manera no podrien recuperar la inversió, però això és una altra raó per la qual no hi ha lliure entrada.
- Assegurança i risc moral: L'existència d'assegurances sanitàries redueix la sensibilitat dels pacients al preu real, podent portar a un consum excessiu (risc moral). Això augmenta els costos per als asseguradors. Quan els proveïdors tenen poder de mercat gràcies a les patents, poden fixar preus encara més alts.
- Prescriptors com a agents: Els metges, com a experts, medien la demanda de medicaments, però sovint no coneixen els preus relatius ni són sensibles a ells. La separació entre prescripció i dispensació, si bé ajuda a evitar problemes d'agència relacionats amb el lucre directe, limita l'elasticitat-preu dels prescriptors.
- Persistència de la informació asimètrica: Encara que la regulació redueix l'asimetria, no l'elimina. És difícil avaluar l'efecte causal d'un tractament en un individu concret. Els metges poden no estar ben informats sobre els nous desenvolupaments. La publicitat també pot influir en la demanda amb efectes ambigus. Els descomptes secrets redueixen la transparència dels preus.
Aquestes condicions creen un entorn propici per a preus molt alts en els medicaments patentats, generant desafiaments pressupostaris per als pagadors. Si els preus no reflecteixen el valor terapèutic, el mercat no envia els senyals adequats per a la direcció de la innovació. Teòricament, la intervenció governamental en la fixació de preus pot millorar els resultats.
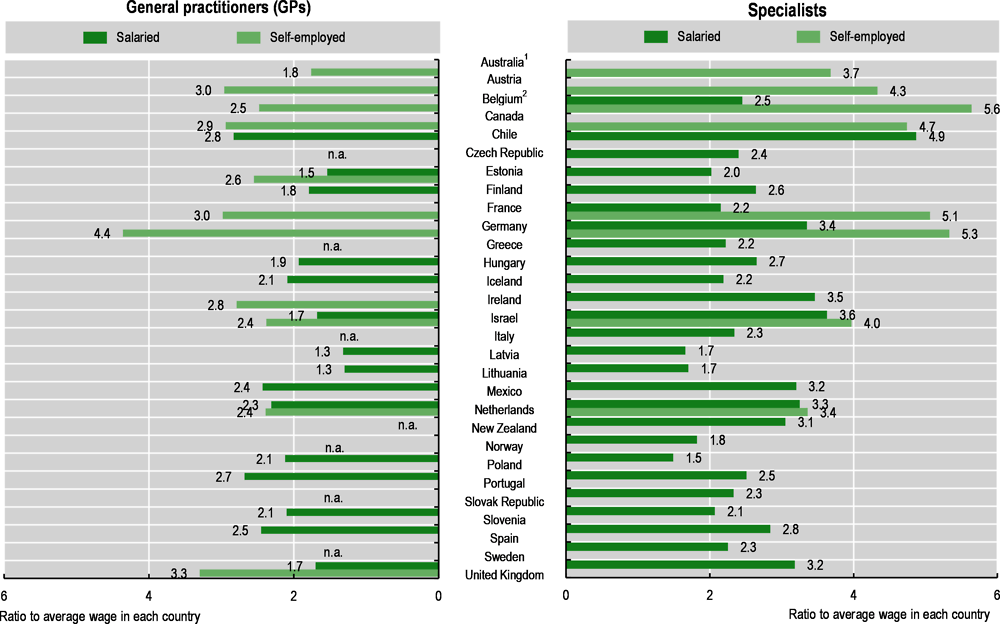
El context dels EUA vs. altres països: Els EUA són una excepció entre els països desenvolupats per tenir un paper més limitat del govern en l'assistència sanitària i la fixació de preus de medicaments. Tot i que els preus dels medicaments són més alts, la despesa total en salut als EUA també és molt més alta. De fet, la proporció de la despesa farmacèutica dins de la despesa total en salut és la més baixa als EUA. Això suggereix que altres components de l'assistència sanitària als EUA (com els salaris de metges i infermeres) són relativament més cars.
Desafiaments de la intervenció governamental: Dissenyar un mercat centralitzat eficient és complex. La fixació de preus de medicaments és inherentment una eina de política d'innovació. Les patents, per si soles, són insuficients si els preus només busquen maximitzar el benestar estàtic; cal alinear el valor social i les recompenses privades per guiar la innovació cap a productes socialment valuosos. Mesurar el valor social d'un fàrmac és molt difícil; els assajos clínics mostren seguretat i eficàcia sota condicions controlades, no el valor terapèutic global.
Externalitats internacionals: Els medicaments són productes globalment comercialitzats. L'arbitratge de preus (comerç paral·lel/reimportació) pot fer que les empreses decideixin no llançar productes en mercats petits amb preus baixos per protegir els beneficis en països grans. Els incentius a la innovació d'un país beneficien a d'altres (efecte "spillover"). Els mercats petits tenen poc incentiu a pagar preus alts, ja que la seva contribució als ingressos globals és petita. Els mercats grans com els EUA estan subjectes al problema del "free-riding" per part d'altres països.
Tipus d'intervencions en altres països: Els governs, com a compradors monopsonistes, tenen un poder considerable. Les polítiques per controlar els preus dels medicaments patentats varien:
- Basades en costos: Regulacions de "cost-plus" o "taxa de retorn". Busquen limitar els beneficis percebuts com excessius. L'esquema del Regne Unit és un exemple de regulació de taxa de retorn a nivell de cartera. Els economistes són generalment escèptics amb aquests mètodes, especialment a nivell de producte, ja que poden recompensar la despesa en R+D ineficient i no lliguen el preu al valor terapèutic. Requereixen dades internes detallades de les empreses, que són difícils d'obtenir.
- Basades en valor: Propugnades per la indústria, on els preus es basen en el valor terapèutic (superioritat terapèutica) sense tenir en compte els costos de R+D o fabricació. Això requereix Avaluacions de Tecnologies Sanitàries (HTA) que van més enllà dels requisits d'autorització de mercat. Les HTA són costoses i consumeixen temps. La manca de coordinació entre països porta a conclusions diferents sobre el valor d'un fàrmac. Encara que s'estableixi la superioritat, queda determinar quant està disposat a pagar el pagador per aquesta millora clínica. França utilitza el SMR (servei mèdic prestat) i l'ASMR (millora del servei mèdic prestat) com a inputs per a la negociació de preus.
- Llindars de cost-efectivitat: Els pagadors utilitzen el seu poder per rebutjar la cobertura si el preu per unitat de benefici per a la salut (com un QALY - Quality-Adjusted Life Year) supera la seva disposició a pagar. El Regne Unit i Alemanya utilitzen avaluacions de cost-efectivitat com a instrument principal. Això també requereix HTA i consens sobre el valor d'una vida estadística.
Punts de referència i comerç paral·lel: Les intervencions sovint utilitzen altres preus com a referència.
- Preus de referència interns: Estableixen el nivell de reemborsament d'un nou producte igual al d'un producte competidor dins del mateix país. Permeten que els pacients paguin una prima per productes preferits, introduint certa sensibilitat al preu. L'eficiència depèn de la informació dels pacients/prescriptors i de l'elecció del producte de referència.
- Preus de referència externs: Comparen el preu del mateix producte en altres països. Molts països europeus l'utilitzen. La motivació principal sembla ser la percepció d'equitat. Un argument en contra important és que incentiva els fabricants a endarrerir el llançament (o no llançar) en els països de preus baixos que s'utilitzen com a referència, ja que el preu en aquests països afecta el preu en els països referenciadors.
- Comerç paral·lel o reimportació: Permet importar medicaments venuts a preus més baixos en altres països. Aquest arbitratge limita la capacitat de les empreses per discriminar preus entre països, la qual cosa els economistes sovint consideren relativament eficient, especialment per facilitar l'accés en països més pobres. Tant els preus de referència externs com el comerç paral·lel no han eliminat completament les diferències de preus entre països. Els preus reals reflecteixen polítiques, preferències i poder de negociació, no només el PIB per càpita.
Possibilitat d'importar polítiques als EUA: El paper més gran del sector privat i la manca de cobertura universal als EUA fan que un mateix fàrmac tingui preus molt diferents per a diferents compradors. Els PBM (Pharmacy Benefit Managers) negocien preus i col·locació al formulari, controlant l'accés a grans poblacions de pacients. A diferència dels pagadors governamentals, els PBM busquen maximitzar beneficis, no el benestar social, i poden no internalitzar els beneficis a llarg termini de la innovació. El govern federal dels EUA, tot i ser un gran pagador, va tenir un paper limitat en la negociació de preus fins recentment.
- Inflation Reduction Act (IRA) de 2022: Va introduir el Programa de Negociació de Preus de Medicaments de Medicare. Estableix un preu màxim just (MFP) per a certs fàrmacs basat en els anys des de l'aprovació, no el valor. Es temen conseqüències no desitjades, com l'endarreriment de llançaments o el "product hopping" (introduir noves versions abans que expiri la patent per evitar la negociació). Atesa la gran mida del mercat dels EUA, les seves polítiques poden afectar significativament la R+D global.
- Propostes per vincular preus als EUA amb els d'altres països: La reimportació des del Canadà s'ha proposat i fins i tot aprovat a nivell estatal per la FDA recentment. No obstant això, és probable que tingui efectes modestos en els preus globals dels EUA a causa de la petita mida del mercat canadenc, i podria reduir l'accés al Canadà. Els preus de referència externs també tenen suport bipartidista, però la indústria s'hi oposa. L'experiència europea suggereix que portaria a respostes estratègiques com l'endarreriment de llançaments i l'ús de descomptes secrets. Aquests preus no públics dificulten les avaluacions econòmiques.
En general, l'adopció de reimportació o preus de referència externs als EUA tindria efectes modestos en els preus dels EUA, però podria reduir l'accés o la transparència en altres països. La negociació de preus de Medicare (IRA) té un potencial més gran per afectar els preus als EUA i la R+D global, però el seu efecte depèn de si es basa en avaluacions de valor fiables.
Enfocaments alternatius: Davant la insatisfacció amb l'statu quo i els reptes pressupostaris que presenten teràpies molt valuoses (com Sovaldi per a l'Hepatitis C o els nous fàrmacs per a l'obesitat), s'estan considerant o experimentant alternatives:
- Contractació abans de la innovació (Ex Ante): Separar les recompenses per la innovació de les vendes amb alt marge, utilitzant pagaments fixos per a la innovació exitosa. Exemples inclouen premis o compromisos de mercat anticipats (AMCs). Els AMCs ofereixen més certesa pressupostària i clars incentius a la innovació. Exemples reals inclouen la vacuna contra el pneumococ finançada per la Fundació Gates i l'Operació Warp Speed per a les vacunes de la COVID-19. Requereixen fer moltes suposicions sota incertesa, cosa que n'explica la raresa. Pateixen del mateix risc de "free-riding" internacional.
- Contractació després de la innovació: Més fàcils d'implementar ja que mantenen el sistema de patents.
- Subhastes: S'utilitzen per a genèrics. Possible per a productes patentats si hi ha substituts propers. Les "patent buyouts" (compra de patents per part del govern per posar la propietat intel·lectual en domini públic) s'han proposat, però la seva aplicació és incerta, especialment a nivell global. Els drets de "march-in" als EUA rarament s'exerceixen.
- Preus de subscripció ("Model Netflix"): Un pagament fix al fabricant per subministrar qualsevol quantitat demandada a un preu zero o proper a zero. Proporciona certesa pressupostària i redueix l'incentiu del fabricant a comercialitzar el producte de manera inapropiada. Els desafiaments inclouen la rigidesa davant nova informació o competidors i la reducció de l'incentiu per trobar nous usos. Austràlia i alguns estats dels EUA l'han implementat per a l'Hepatitis C amb resultats mixts.
- Contractes basats en resultats ("Pay-for-performance", "Risk-sharing"): Vinculen els pagaments a la realització de fites clíniques futures. Aborden la informació imperfecta al llançament sense endarrerir l'accés i alineen els incentius del fabricant amb els resultats del pacient. No obstant això, la seva adopció es veu limitada per la dificultat de negociar-los, la manca d'evidència sobre els resultats, la infraestructura de dades insuficient i els desafiaments de mesura.
Context més ampli de la despesa sanitària: L'article conclou que, tot i l'atenció que reben els preus dels medicaments, no semblen ser el principal impulsor de l'augment total dels costos sanitaris als EUA o altres països d'ingressos alts. La competència de genèrics als EUA és generalment robusta, amb ràpida entrada i caigudes de preus després de l'expiració de patents. Els marges baixos en molts genèrics han portat a l'abandonament de fabricants i escassetats, especialment per a injectables. Els preus dels genèrics als EUA són més baixos que en països similars.
Les grans companyies farmacèutiques als EUA tenen marges de benefici i despesa en R+D significativament més alts que altres indústries. Aquesta R+D es fa amb l'expectativa de beneficis futurs. Les polítiques que redueixen els beneficis esperats disminueixen la R+D i la innovació. La mida del mercat dels EUA fa que les seves decisions polítiques siguin molt més influents en la innovació global. Les polítiques que recompensen específicament la innovació més important (com els fàrmacs orfes) semblen més exitoses. Les pròpies empreses tenen dificultats per identificar els productes més rendibles a causa del risc tècnic i de mercat, i la manca de claredat dels pagadors pot contribuir a la incertesa.
Per millorar els resultats, els responsables polítics haurien de centrar-se no només a reduir el preu mitjà o la despesa total, sinó també a acceptar preus més alts per a fàrmacs efectius, reduint les recompenses per teràpies ineficaces, i valorant els beneficis a llarg termini. Abordar les friccions i imperfeccions del mercat és crucial per augmentar l'eficiència.