Measuring the health-related Sustainable Development Goals in 188 countries: a baseline analysis from the Global Burden of Disease Study 2015
27 de setembre 2016
20 de setembre 2016
Who's affraid of economic evaluation?
El disseny institucional de l'avaluació econòmica
L'avaluació de polítiques públiques en l'àmbit sanitari: la millora de l'atenció a l’ictus a Catalunya com a exemple
Today I'll suggest a reading from the latest issue of Nota d'Economia. You'll find two articles of special interest for health economists. The first one, on institutional design will convince you that this is the tough part of the issue. Governments prefer to avoid difficult decisions, only a proper institucional design will provide the best impact of economic evaluation. The second one is an excellent example of the impact of stroke prevention and care, or how organizational innovation may deliver social value of 372M€ in 7 years. Great, we need more initiatives like that, and studies that assess its impact.
This is the summary:
PS. US is affraid of economic evaluation...have a look at JAMA
L'avaluació de polítiques públiques en l'àmbit sanitari: la millora de l'atenció a l’ictus a Catalunya com a exemple
Today I'll suggest a reading from the latest issue of Nota d'Economia. You'll find two articles of special interest for health economists. The first one, on institutional design will convince you that this is the tough part of the issue. Governments prefer to avoid difficult decisions, only a proper institucional design will provide the best impact of economic evaluation. The second one is an excellent example of the impact of stroke prevention and care, or how organizational innovation may deliver social value of 372M€ in 7 years. Great, we need more initiatives like that, and studies that assess its impact.
This is the summary:
Aquest estudi mostra que després de les millores que han tingut lloc en l’atenció a l’ictus agut a Catalunya (Abilleira et al., 2009, 2011a, 2011b; Salvat-Plana et al., 2011) en el període 2005-2012 es van evitar 719 defuncions i es van guanyar 11.153 anys de vida, amb un valor social mínim de 353.164.622,08 euros (1.050.147.483,07 euros màxim). Un cop eliminat l’efecte de l’augment de la incidència, el nombre de defuncions per ictus va ser de 919 i 11.760 anys de vida guanyats, amb un valor social mínim de 372.404.624,76 euros (1.195.167.115,79 màxim)
PS. US is affraid of economic evaluation...have a look at JAMA
Neus Martin
18 de setembre 2016
The anxiety of inaccuracy
Conflicting Interpretation of Genetic Variants and Cancer Risk by Commercial Laboratories as Assessed by the Prospective Registry of Multiplex Testing
What happens if "one quarter of the clinical genetic results from commercially available multiplex cancer panels and reported at the PROMPT registry had conflicting interpretations" and if "36% of conflicting genetic tests results appeared to be clinically relevant, because they were either reported as pathogenic/likely pathogenic"? Does anybody care about it?.
I would suggest today you have a look at this article and your level of anxiety will increase suddenly.
PS. On genetic testing
What happens if "one quarter of the clinical genetic results from commercially available multiplex cancer panels and reported at the PROMPT registry had conflicting interpretations" and if "36% of conflicting genetic tests results appeared to be clinically relevant, because they were either reported as pathogenic/likely pathogenic"? Does anybody care about it?.
I would suggest today you have a look at this article and your level of anxiety will increase suddenly.
Clinical data and genetic testing results were gathered from1,191 individuals tested for inherited cancer susceptibility and self-enrolled in PROMPT between September 2014 and October 2015. Overall,participants (603 genetic variants) had a result interpreted by more than one laboratory, including at least one submitted to ClinVar, and these were used as the final cohort for the current analysis.Therefore,
Of the 603 variants, 221 (37%) were classified as a variant of uncertain significance (VUS), 191 (32%) as pathogenic, and 34 (6%) as benign. The interpretation differed among reporting laboratories for 155 (26%). Conflicting interpretations were most frequently reported for CHEK2 and ATM, followed by RAD51C, PALB2, BARD1, NBN, and BRIP1. Among all participants, 56 of 518 (11%) had a variant with conflicting interpretations ranging from pathogenic/likely pathogenic to VUS, a discrepancy that may alter medical management.
Clinical interpretation of genetic testing for increased cancer susceptibility as assessed by multiplex panels hinges on accurate curation and interpretation of variants. Discrepant interpretation of some genetic variants appears to be common.Take care. The regulator remains on vacation, a never ending vacation.
PS. On genetic testing
16 de setembre 2016
The costs of inaccuracy
The
Lifetime Economic Burden of Inaccurate HER2 Testing: Estimating the
Costs of False-Positive and False-Negative HER2 Test Results in US
Patients with Early-Stage Breast Cancer
Diagnostic tests show different levels of false positive and negatives in the results. The impact of such unwanted results by physicians finally have an impact on health and quality of life of patients. You can check what does this means for HER-2 test in breast cancer in US in this article.
However, as Kassirer said:
Diagnostic tests show different levels of false positive and negatives in the results. The impact of such unwanted results by physicians finally have an impact on health and quality of life of patients. You can check what does this means for HER-2 test in breast cancer in US in this article.
Patients with breast cancer whose tumors test positive for human epidermal growth factor receptor 2 (HER2) are treated with HER2-targeted therapies such as trastuzumab, but limitations with HER2 testing may lead to false-positive (FP) or false-negative (FN) results.That's a lot. Something should be done to improve accuracy in such tests. It was already known partially. Its cost-effectiveness is sensitive to HER-2 test properties.
Among 226,870 women diagnosed with EBC in 2012, 3.12% (n = 7,070) and 2.18% (n = 4,955) were estimated to have had FP and FN test results, respectively. Approximately 8400 QALYs (discounted, lifetime) were lost among women not receiving trastuzumab because of FN results. The estimated incremental per-patient lifetime burden of FP or FN results was $58,900 and $116,000, respectively. The implied incremental losses to society were $417 million and $575 million, respectively.
However, as Kassirer said:
Absolute certainty in diagnosis is unattainable, no matter how much information we gather, how many observations we make, or how many tests we perform. A diagnosis is a hypothesis about the nature of a patient's illness, one that is derived from observations by the use of inference. Our task is not to attain certainty, but rather to reduce the level of diagnostic uncertainty enough to make optimal therapeutic decisions.That's it.
Rafel Joan
12 de setembre 2016
The US political gridlock on cost-effectiveness
A Framework for Payer Assessment of the Value of New Technologies:A US Approach
USA is well known for its prominent interest in avoiding cost-effectiveness as we know in certain european countries. They talk about comparative effectiveness research, because it fits with their current priorities: What works best? and let's the cost for another day. Forget trade-offs.
If you want to know the recent stuff on the topic, have a look at this article. You'll notice three steps: clinical care value, managing affordability and health system value. It makes sense as a first step. In our country we don't have such official estimates. The next step should be to introduce cost and equity considerations.
USA is well known for its prominent interest in avoiding cost-effectiveness as we know in certain european countries. They talk about comparative effectiveness research, because it fits with their current priorities: What works best? and let's the cost for another day. Forget trade-offs.
If you want to know the recent stuff on the topic, have a look at this article. You'll notice three steps: clinical care value, managing affordability and health system value. It makes sense as a first step. In our country we don't have such official estimates. The next step should be to introduce cost and equity considerations.
Xavier Rodés
07 de setembre 2016
A healthcare expenditure mess, and nobody cares about it
Let's imagine an alleged State. All its citizens pay taxes under the same Tax Code. Health Benefits are the same under the Health Act. And spending on health care according to geography, can reach 52% more in Basque country compared to Andalusia. This is not new. Many decades having the same figure and nobody cares about it.
 This is an easy table to understand health policy making in a failed state. Catalonia spends 4,7% of GDP on health, other sources say 5,5%. Anyway, you'll not find an OECD country with similar figures. After a decade we are spending the same amount per citizen than in 2006, 1.120 €. I will not add anything to this mess. There is only an increasing need to disconnect. Is there any MP in the room?
This is an easy table to understand health policy making in a failed state. Catalonia spends 4,7% of GDP on health, other sources say 5,5%. Anyway, you'll not find an OECD country with similar figures. After a decade we are spending the same amount per citizen than in 2006, 1.120 €. I will not add anything to this mess. There is only an increasing need to disconnect. Is there any MP in the room?
 This is an easy table to understand health policy making in a failed state. Catalonia spends 4,7% of GDP on health, other sources say 5,5%. Anyway, you'll not find an OECD country with similar figures. After a decade we are spending the same amount per citizen than in 2006, 1.120 €. I will not add anything to this mess. There is only an increasing need to disconnect. Is there any MP in the room?
This is an easy table to understand health policy making in a failed state. Catalonia spends 4,7% of GDP on health, other sources say 5,5%. Anyway, you'll not find an OECD country with similar figures. After a decade we are spending the same amount per citizen than in 2006, 1.120 €. I will not add anything to this mess. There is only an increasing need to disconnect. Is there any MP in the room?
PS. I'm not arguing that every country has to spend the same, I'm just saying that it is not legally possible to deliver the same benefits with such different budgets. Therefore we are unequal before law. This is the usual legal uncertainty of a failed state.
06 de setembre 2016
Physicians' standards of conduct
Professing the Values of MedicineThe Modernized AMA Code of Medical Ethics
JAMA has decided to start JAMA Professionalism, a new department.
A multi-year effort to modernise that has provided an interesting outcome. You can check for example, regarding prioritisation of resources, what should be done? in chapter 11 you'll find the answers. A good suggestion for our physicians' associations and their outdated codes.
JAMA has decided to start JAMA Professionalism, a new department.
The goal of the articles in this section is to help physicians fulfill required competencies on this topic. According to the American Board of Medical Specialties definition, professionalism is “…a commitment to carrying out professional responsibilities, adherence to ethical principles and sensitivity to diverse patient populations.” Taking responsibility for executing professional responsibility seems intuitive enough. But what does it mean to adhere to ethical principles? How are the ethical principles defined?Good questions. And the answers for US physicians are in the new AMA Code of Medical Ethics.
A multi-year effort to modernise that has provided an interesting outcome. You can check for example, regarding prioritisation of resources, what should be done? in chapter 11 you'll find the answers. A good suggestion for our physicians' associations and their outdated codes.
02 de setembre 2016
Predictive modeling in health care (2)
Analysing the Costs of Integrated Care: A Case on Model Selection for Chronic Care Purposes
How do you want to manage, with a rearview mirror or just looking forward? Big data allows to look forward with better precision. The uncertainty about the disease and about the cost of care is large when you enter in hospital from an emergency department. But, after the diagnosis (morbidity), could we estimate how much could cost an episode?. If so, then we could compare the expected cost and the observed cost on a continous process.
Right now this is possible. Check this article that we have just published and you'll understand that costs of different services according to morbidity can be reckoned and introduced in health management. This analysis goes beyong our former article, much more general. So, what are we waiting for? Big data is knocking at the door of health care management, predictive modeling is the tool.
How do you want to manage, with a rearview mirror or just looking forward? Big data allows to look forward with better precision. The uncertainty about the disease and about the cost of care is large when you enter in hospital from an emergency department. But, after the diagnosis (morbidity), could we estimate how much could cost an episode?. If so, then we could compare the expected cost and the observed cost on a continous process.
Right now this is possible. Check this article that we have just published and you'll understand that costs of different services according to morbidity can be reckoned and introduced in health management. This analysis goes beyong our former article, much more general. So, what are we waiting for? Big data is knocking at the door of health care management, predictive modeling is the tool.
Amazing concert by Caravan Palace in Sant Feliu de Guixols three weeks ago.
01 d’agost 2016
Summer readings
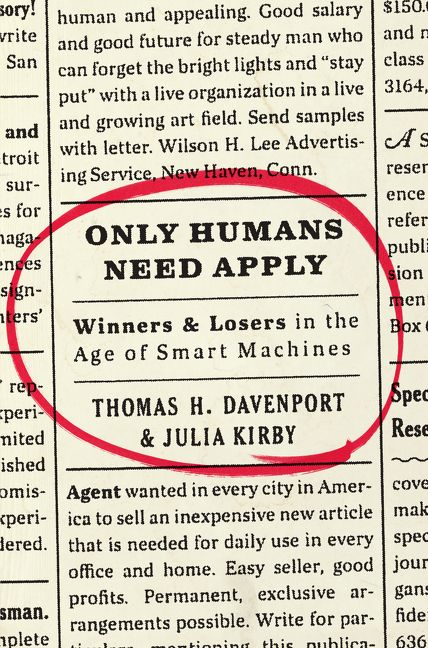
FT published its list some weeks ago. Have a quick look at it, you'll find worthy material. Two selected picks:
and my recommendation:
Have a good summer!
and my recommendation:
Have a good summer!
28 de juliol 2016
The dark side, the conflict option
The dark side of the force
While reading today FM Alvaro op-ed on current war: Questions in a war, I thought that was good to remember Jack Hirshleifer and specifically to retrieve an excellent speech he gave in 1993: The dark side of the force. When I read it for the first time I got impressed and I've remembered forever.
Therefore, my suggestion is to read the whole speech. If you are an economist, you'll be shaken by his views. Selected statements:
Hirshleifer analytic frame may be applied to health economics as well, specifically to such cases where fraud, inappropriateness, and false advertising are part of the dark force.
PS. Long time ago I quoted in a post the Schelling book on the same topic.
While reading today FM Alvaro op-ed on current war: Questions in a war, I thought that was good to remember Jack Hirshleifer and specifically to retrieve an excellent speech he gave in 1993: The dark side of the force. When I read it for the first time I got impressed and I've remembered forever.
Therefore, my suggestion is to read the whole speech. If you are an economist, you'll be shaken by his views. Selected statements:
“Our profession has on the whole taken not too harsh but rather too benign a view of the human enterprise. Recognizing the force of self-interest, the mainline Marshallian tradition has nevertheless almost entirely overlooked what I will call the dark side of the force—to wit, crime, war, and politics."
“cooperation, with a few obvious exceptions, occurs only in the shadow of conflict.” “when people cooperate, it is generally a conspiracy for aggression against others (or, at least, is a response to such aggression).”
"Pareto is saying, sure, you can produce goods for the purpose of mutually beneficial exchange with other parties—OK, that's Marshall's "ordinary business." But there's another way to get rich: you can grab goods that someone else has produced. Appropriating, grabbing, confiscating what you want— and, on the flip side, defending, protecting, sequestering what you already have—that's economic activity too. Take television. Cops chase robbers, victims are stalked by hitmen (or should I say hitpersons?), posses cut off rustlers at the pass, plaintiffs sue defendants, exorcists cast spells against vampires. What is all this but muscular economics? Robbers, rustlers, hitpersons, litigants—they're all trying to make a living. Even vampires are making economic choices: sucking blood is presumably the cost-effective way of meeting their unusual nutritional needs.”
“This is Machiavelli's version of the golden rule: he who gets to rule, will get the gold. Human history is a record of the tension between the way of Niccolo Machiavelli and what might be called the way of Ronald Coase. According to Coase's Theorem, people will never pass up an opportunity to cooperate by means of mutually advantageous exchange. What might be called Machiavelli’s Theorem states that no one will ever pass up an opportunity to gain a one-sided advantage by exploiting another party.
Machiavelli's Theorem standing alone is only a partial truth, but so is Coase's Theorem standing alone. Our textbooks need to deal with both modes of economic activity. They should be saying that decision-makers will strike an optimal balance between the way of Coase and the way of Machiavelli—between the way of production combined with mutually advantageous exchange, and the dark-side way of confiscation, exploitation, and conflict.”
"Thus, in recognizing the role of conflict we must not go overboard in the other direction. All aspects of human life are responses not to conflict alone, but to the interaction of the two great life-strategy options: on the one hand production and exchange, on the other hand appropriation and defense against appropriation. Economics has done a great job in dealing with the way of Ronald Coase; what we need now is an equally subtle and structured analysis of the dark side: the way of Niccolo Machiavelli.”
The balance between these modes of economic activity--the one leading to greater aggregate wealth, and the other to conflict over who gets the wealth--provides the main story line of human history.This speech and several articles on conflict were published in a book "The Dark Side of the Force: Economic Foundations of Conflict Theory".
Hirshleifer analytic frame may be applied to health economics as well, specifically to such cases where fraud, inappropriateness, and false advertising are part of the dark force.
PS. Long time ago I quoted in a post the Schelling book on the same topic.
27 de juliol 2016
DNA methylation assays as epigenetic biomarkers
Quantitative comparison of DNA methylation assays for biomarker development and clinical applications
A new milestone has been achieved in Medicine. Tracking epigenetic alterations is crucial to understand a disease. However, epigenetic biomarkers are needed to assess such changes. Its precision (sensitivity-specifity) is paramount for its clinical application. Now a group of international researchers has certified its performance (partially). Have a look at this Nature article:
PS. Neuroepigenetics: DNA methylation and memory
A new milestone has been achieved in Medicine. Tracking epigenetic alterations is crucial to understand a disease. However, epigenetic biomarkers are needed to assess such changes. Its precision (sensitivity-specifity) is paramount for its clinical application. Now a group of international researchers has certified its performance (partially). Have a look at this Nature article:
Genome-wide mapping and analysis of DNA methylation has become feasible for patient cohorts with thousands of samples, and epigenome-wide association studies have been conducted for numerous biomedically relevant phenotypes. To translate relevant epigenome associations into clinically useful biomarkers, it is necessary to select a manageable set of highly informative genomic regions, to target these loci with DNA methylation assays that are sufficiently fast, cheap, robust and widely available to be useful for routine clinical diagnostics, and to confirm their predictive value in large validation cohorts.Among its conclusions I would like to highlight three of them:
(i) Absolute DNA methylation assays are the method of choice when validating DNA methylation differences in large cohorts, and they are also an excellent technology for developing epigenetic biomarkers.
(ii) Relative DNA methylation assays are not a good replacement for absolute assays. However, experiences of scientists in the contributing laboratories suggest that carefully selected, designed and validated relative assays can cost-effectively detect minimal races of methylated DNA against an excess of unmethylated DNA.
(iii) Global DNA methylation assays suffer from noisy data and divergent results between technologies. Locus-specific assays (possibly combined with prediction) provide a more robust alternativeThat's it. Very soon will see the epigenetic biomarkers in routine clinical use. And afterwards, epigenetic drugs and treatments. Then, we'll confirm that the promise of precision medicine is a reality. The implications for medicine as a scientific discipline and clinical decision making are huge, and specifically, healthcare organizations will need to adapt to new knowledge and technologies.
PS. Neuroepigenetics: DNA methylation and memory
06 de juliol 2016
Food and risk perception
Food and the Risk Society: The Power of Risk Perception
This is the main message of the book: Do not send generic messages on food and its risks, the time for segmentation has arrived,
This is the main message of the book: Do not send generic messages on food and its risks, the time for segmentation has arrived,
A generic approach, involving the provision of vast amounts of information to the general public, stands a real risk of leading to information overload, bewilderment and lack of interest among mainstream consumers. A more effective approach to change consumer food buying and consumption behaviour, is to focus on segmenting the population according to their information needs, and developing information with high levels of personal relevance to specific groups of respondents who may be at greater risk than the rest of the population. Such information is more likely to create attitudinal change and subsequent behavioural change as the perceived personal relevance is high.Is the government already prepared for the task?
03 de juliol 2016
Voluntary health insurance, it's role and regulation
Voluntary health insurance in Europe: Role and regulation
Voluntary health insurance in Europe: country experience
A long time has passed since WHO published a book on voluntary health insurance, just a decade (!). Therefore, there are many reasons to review again what's going on, and this is precisely what you'll find in two recent books.
Before any recommendation, it is good to have a good analysis. And the best analysis comes from reliable data. Somebody should check the published data in the book. In the case of Spain it says 10% of suplementary insurance, while it is around 16% (!) (p.50) (and it is duplicate really according to OECD classfication). And beyond that, it says that there is 3% of voluntary health insurance that is substitutive, while it is exactly 0% (!). Therefore take care. I'll not comment anything else.
Voluntary health insurance in Europe: country experience
A long time has passed since WHO published a book on voluntary health insurance, just a decade (!). Therefore, there are many reasons to review again what's going on, and this is precisely what you'll find in two recent books.
Before any recommendation, it is good to have a good analysis. And the best analysis comes from reliable data. Somebody should check the published data in the book. In the case of Spain it says 10% of suplementary insurance, while it is around 16% (!) (p.50) (and it is duplicate really according to OECD classfication). And beyond that, it says that there is 3% of voluntary health insurance that is substitutive, while it is exactly 0% (!). Therefore take care. I'll not comment anything else.
01 de juliol 2016
Why is it useless to predict future health expenditures?
National spending on health by source for 184 countries between 2013 and 2040
The Lancet has just published a new estimate of the size of health expenditures in the future up to 2040. Too often nobody looks backward and check what predictions said before. If somebody does it, it will get a surprise for the first time, however the following ones he will convey that predictions are useless, because there are too many uncertain situations to take into account. Basically most of the hypothesis are flawed. Take this statement from the article:
The Lancet has just published a new estimate of the size of health expenditures in the future up to 2040. Too often nobody looks backward and check what predictions said before. If somebody does it, it will get a surprise for the first time, however the following ones he will convey that predictions are useless, because there are too many uncertain situations to take into account. Basically most of the hypothesis are flawed. Take this statement from the article:
Despite remarkable health gains, past health fnancing trends and relationships suggest that many low-income and lower-middle-income countries will not meet internationally set health spending targets and that spending gaps between low-income and high-income countries are unlikely to narrow unless substantive policy interventions occur. Although gains in health system efficiency can be used to make progress, current trends suggest that meaningful increases in health system resources will require concerted action.Is there anybody that can tell me what "internationally set health spending targets" are?. Who sets them?. If anybody wants to check what I'm saying, have a look at the cutbacks from the great recession and the estimates by OECD or EU. Everybody was saying that technology innovation and aging would boost health expenditures forever, and now we know that this is not true. Forget the article. Distrust the fortune-tellers.
Subscriure's a:
Missatges (Atom)