MODERN MONOPOLIES: What It Takes to Dominate the 21st-Century Economy
Platform business is the hottest topic in organizational economics. Linear business considered as a traditional value chain is exactly the opposite of the economics of platforms. Two years ago I explained in
several posts the emergence of this model. In 2004
Tirole and Rochet defined the network externalities that emerged from multisided platforms. Nowadays it is the hottest topic and
a new book explains the consequences.
The secret to tech companies’ success lies not in the tech, but in it’s business model. A platform, by definition, creates value by facilitating an exchange between two or more interdependent groups. So, rather than making things, they simply connect people. The book helps you understand what made these companies so successful, how to tell a good platform from the bad, and how you could build one too
And by definition, platforms are the new modern monopolies different from the ones we have known.
Although monopolies get a bad rap, they’re not always a bad thing. In the short term, modern monopolies are often a boon to consumers. They bring valuable new inventions to market, and, in the case of platforms, they build new communities and markets that would not exist otherwise. The downside comes much later, as the monopolist ages and starts to crowd out potential new competitors without delivering new value.
Today
Amazon is the most valuable company in the world. That's it. Let's wait for the downside. It may be too late to react.
Regulators should read today Jean Tirole and apply his recommendations.
PS. Go to the conclusion and you'll find this statement:
So where should you be looking to next? Well, there are a few industries where the three factors are starting to converge
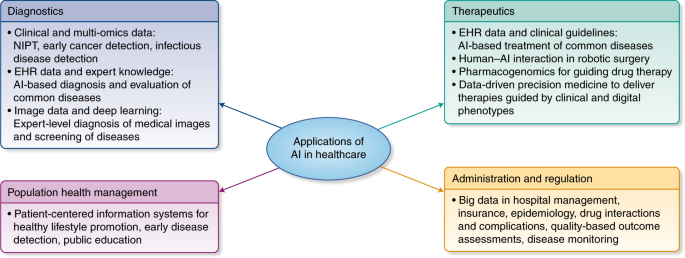
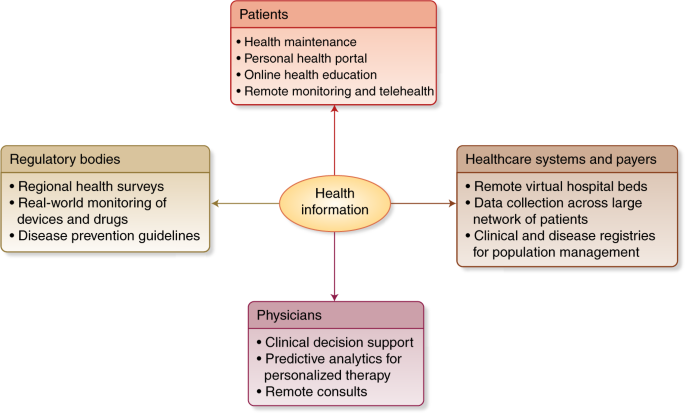
The first industry is health care, which we’ve touched on at several points in this book. Here you have platforms connecting doctors and patients in new ways, like Doctor on Demand, Teladoc, and ZocDoc. However, these platforms are just going after the low-hanging fruit. There’s still a tremendous amount of waste and inefficiency in the healthcare sector, especially in the United States. And wherever there’s waste and inefficiency, there’s a platform opportunity. For instance, although they’re relatively popular with casual consumers, wearable health devices are just starting to make their way into formal health care. These devices offer tremendous potential for improving patient wellness. But in order for them to be useful, a platform will need to build a unified network of doctors and patients. Despite the recent entrance of Silicon Valley heavyweights Apple and Google, this market is still wide open.
PS. Four additional useful books on the same topic:
Evans and Schmalensee are the best authors on this subject and this is the recommended book for economists.
A historical perspective on platforms.
A book that connects platforms with other topics of interest.
A
management perspective on platforms.