THE COVID-19 CRISIS. Social Perspectives
In Chapter 13
13 Post-pandemic Routes in the Context of Latin Countries: The Impact of COVID-19 in Italy and Spain by Anna Sendra, Jordi Farré, Alessandro Lovari and Linda Lombi
In terms of health and risk communication, the COVID crisis has emphasised the lack of specific training in crisis and emergency communication of many public sector organisations, including health institutions. This first social media pandemic has been a major challenge for health communicators; individuals often failed in effectively communicating data and numbers to counteract the infodemic and thus reduce the impact of false narratives. With the increasing diversification of social media platforms, ‘individuals’ health […] will be shaped by a multitude of social forces, each of which can mediate different kinds of health contagion processes’ (Zhang and Centola, 2019). Mitigating the spread of fake news seems to involve coordinated efforts between authorities, mass media and digital companies, but it also appears crucial to invest in education and digital literacy for developing a critical awareness of the use of digital technologies that could be useful for facing future health crises. In other words, the strengthening of comprehensive population-centred responses lies on finding answers concerning how the mechanisms of public concern will operate to engage in coherent protection rules or in what ways the forms of interaction will change
Outline of the book:
PART I: INTRODUCTION
1 COVID Society: Introduction to the Book
Deborah Lupton and Karen Willis
2. Contextualising COVID-19: Sociocultural Perspectives on Contagion
Deborah Lupton
PART II: SPACE, THE BODY AND MOBILITIES
3. Moving Target, Moving Parts: The Multiple Mobilities of the COVID-19 Pandemic
Nicola Burns, Luca Follis, Karolina Follis and Janine Morley
4. Physical Activity and Bodily Boundaries in Times of Pandemic
Holly Thorpe, Julie Brice and Marianne Clark
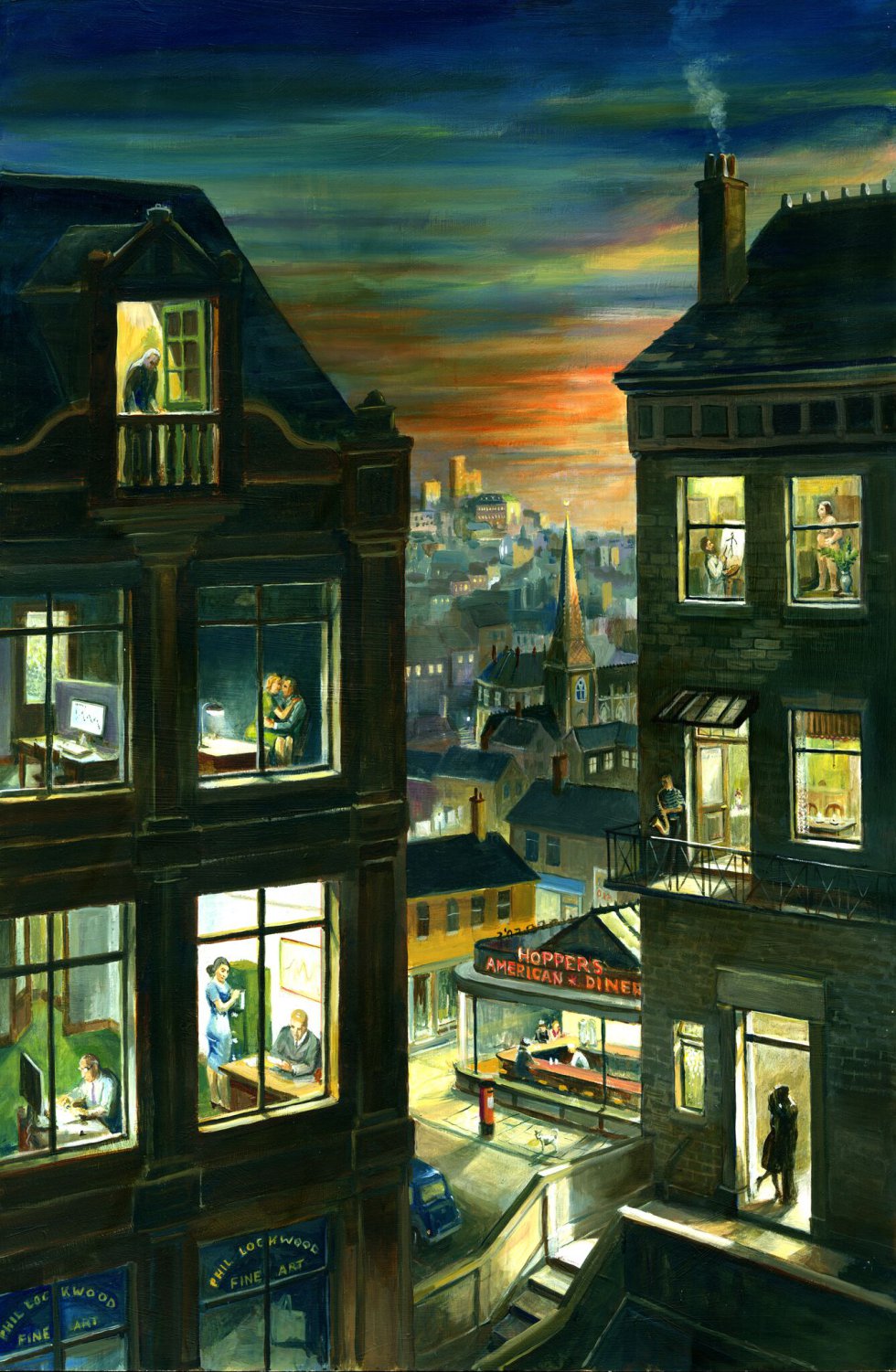
5. City Flows During Pandemics: Zooming in on Windows
Oimpia Mosteanu
6. The Politics of Touch-Based Help for Visually Impaired Persons During the COVID-19 Pandemic: An Autoethnographic Account
Hidi Lourens
PART III: INTIMACIES, SOCIALITIES AND CONNECTIONS
7. #DatingWhileDistancing: Dating Apps as Digital Health Technologies During the COVID-19 Pandemic
David Myles, Stefanie Duguay and Christopher Dietzel
8. ‘Unhome’ Sweet Home: The Construction of New Normalities in Italy During COVID-19
Veronica Moretti and Antonio Maturo
9. Queer and Crip Temporalities During COVID-19: Sexual Practices, Risk and Responsibility
Ryan Thorneycroft and Lucy Nicholas
10. Isol-AID, Art and Wellbeing: Posthuman Community Amid COVID-19
Marissa Willcox, Anna Hickey-Moody and Anne M. Harris
PART IV: HEALTHCARE PRACTICES AND SYSTEMS
11. Strange Times in Ireland: Death and the Meaning of Loss Under COVID-19
Jo Murphy-Lawless
12. Between an Ethics of Care and Scientific Uncertainty: Dilemmas of General Practitioners in Marseille
Romain Lutaud, Jeremy K. Ward, Gaëtan Gentile and Pierre Verger
13 Post-pandemic Routes in the Context of Latin Countries: The Impact of COVID-19 in Italy and Spain
Anna Sendra, Jordi Farré, Alessandro Lovari and Linda Lombi
14. Risky Work: Providing Healthcare in the Age of COVID-19
Karen Willis and Natasha Smallwood
PART V: MARGINALISATION AND DISCRIMINATION
15. The Plight of the Parent-Citizen? Examples of Resisting (Self-)Responsibilisation and Stigmatisation by Dutch Muslim Parents and Organisations During the COVID-19 Crisis
Alex Schenkels, Sakina Loukili and Paul Mutsaers
16. Anti-Asian Racism, Xenophobia and Asian American Health During COVID-19
Aggie J. Yellow Horse
17. Ageism and Risk During the Coronavirus Pandemic
Peta S. Cook, Cassie Curryer, Susan Banks, Barbara Barbosa Neves, Maho Omori, Annetta H. Mallon and Jack Lam