17 de gener 2021
05 d’abril 2020
Security policies in front of a new molecular vision of life
The goal of this book in one sentence:
This volume reveals the major challenges involved in securing populations pharmaceutically and explores how governments are designing extensive new medical countermeasure regimes to overcome those challenges. At the heart of this pharmaceutical turn in security policy, I argue, lies something deeper: the rise of a new molecular vision of life that is reshaping the world we live in—including the way we now imagine and practice security.The author explains the pharmaceutical defenses for a global pandemic, and specially describes the case of Tamiflu.
The idea of “medical countermeasures” is also fascinating, secondly, because of the terminology it musters. The concept textually embodies the progressive epistemic fusion of the two professional fields of medicine (“medical”) and security (“countermeasures”), attempting to seamlessly blend key vocabularies from both communities into a single notion. Here the term begins to form a fascinating intersection, or bridge, between these two different social fields, giving rise in the process to a fascinating new and interdisciplinary policy space where the respective concerns of pharmaceuticals and security begin to interpenetrate each other, and can also come into direct tension with one another.The chapter 4 is specially of interest: The Margin Call for Regulatory Agencies and explains what was done in the Tamiflu case.
A cursory review of the FDA approval processes for Tamiflu paints a fairly uneventful picture. In fact, the sequence of events leading up to FDA approval for Tamiflu can be quickly summarized. A month after the Swiss approval, on 27 October 1999, the FDA approved Tamiflu for “the treatment of uncomplicated acute illness due to influenza infection in adults who have been symptomatic for no more than 2 days” (FDA 1999b). This marketing approval process unfolded rapidly according to the priority review procedure—within six months—following Roche’s initial application for FDA approval on 29 April 1999.
Again, the case of Tamiflu has been highly instructive. It showed that this new pharmaceutical intervention could only be designed after scientists had first gained a much better understanding of the precise molecular processes involved in viral replication unfolding inside the human body—especially the role played by the influenza virus’s surface proteins such as neuraminidase. Once scientists had understood the vital role played by the neuraminidase and decoded its precise molecular structure, they discovered a “static” site that could form the basis for a new drug target. Scientists could then set about the task of deliberately designing an “artificial” molecule that would bind to that critical site in the neuraminidase and that could inhibit its key role in the process of viral replication. In that sense, our technical ability to develop new pharmaceutical defenses is itself dependent upon a prior—and deeper—scientific understanding of the life processes unfolding at the scale of the molecular.The case of covid-19 began without any countermeasure, because molecular knowledge started mid-January once it was sequenced. Nowadays, we can only wait for a successful vaccine and therapy.
18 de desembre 2020
How plagues end
From the book:
After its dramatic initial appearance, SARS-2 will ultimately become endemic; it will regularly circulate among us at some low, steady level. This is connected to the second kind of end, which we have already considered: herd immunity. Here, the pathogen is still around, but it has a much more difficult time reestablishing itself. This resembles a well-vaccinated population for any infectious disease; there are only occasional, small outbreaks among nonimmune people.
By 2022 or so, we will reach this outcome naturally or via vaccination. Of course, if we do rapidly develop and distribute a safe and effective vaccine, we could reach herd immunity with fewer deaths. Based on the fundamental R0 of SARS-2, as we saw in chapter 2, up to an estimated 60 to 67 percent of the population could be affected (or roughly two hundred million people in the United States). The necessary percentage could be lower, closer to 40 to 50 percent, given that social network structure means that different people spread the virus to different extents (as we also saw in chapter 2); or it could be higher, if the epidemic moves extremely fast and we overshoot the level required for herd immunity. Whatever the exact percentage, as a pathogen spreads, some people will die and others will recover and become immune, so eventually the virus will run out of places to go. This is the ordinary, natural way that, biologically speaking, epidemics end.
This is what we mean when we say that a pathogen is under control. But sometimes, plagues are so devastating that a society never recovers. It’s very important to emphasize that, as bad as COVID-19 is, it’s not remotely as bad as epidemics of bubonic plague, cholera, or smallpox that have killed much larger fractions of the population and that have had much larger and longer-lasting effects. Those types of plagues are even associated with the iconography of the Four Horsemen of the Apocalypse, Pestilence riding side by side with War, Famine, and Death. Those epidemics vindicated the adage that “too few of the living were left to bury the dead.”
N. Christakis says at the begining of the book
The god Apollo, for example, was both a healer and the bringer of disease. During the Trojan War, with his silver bow and quiver of arrows, he rained a plague down on the Greeks to punish them for kidnapping and enslaving Chryseis, the daughter of one of his favored priests.
I found myself thinking again about Apollo and his vengeance as I contemplated our own twenty-first-century barrage more than three thousand years after the events described in The Iliad. It seemed to me that the novel coronavirus was a threat that was both wholly new and deeply ancient. This catastrophe called on us to confront our adversary in a modern way while also relying on wisdom from the past.
Excerpts from the last chapter, How plagues end:
The pathogens evolve to respond to us, but we, at a slower pace, also evolve to respond to them. Infectious diseases have been a part of our evolutionary history for so long that they have left a mark on our genes. For instance, humans have evolved genetic changes that have proven useful in coping with malaria beginning over one hundred thousand years ago, tuberculosis over nine thousand years ago, cholera and bubonic plague over six thousand years ago, and smallpox over three thousand years ago.36
Infectious pathogens (even if nonepidemic) have arguably been a crucial selective pressure throughout the evolution of our species.37 The primary killers of human beings across evolutionary time are other human beings. Humans do not have any natural predators that substantially affect survival.38 Except for our microscopic enemies.
The SARS-2 virus is a lot less lethal to people of reproductive age and can be combated with the lifesaving tools of modern medicine, so the impact on human evolution is surely going to be minimal. But, at least in theory, another way epidemics end is that hosts evolve to be resistant. And in fact, we may already have naturally occurring genetic variation in our species that affects the severity of COVID-19 in different populations, which would lay the groundwork for such evolution. Over generations, this can result in changes to the genetic makeup of the afflicted populations.
This social construction of COVID-19 means that the end of the pandemic can also be socially defined. In other words, plagues can end when everyone believes they are over or when everyone is simply willing to tolerate more risk and live in a new way. If everyone willingly risks infection and resumes a semblance of normal life (or, implausibly, if everyone decides to employ physical distancing forever), then the epidemic can be said to have ended, even if the virus is still circulating. We got a glimpse of this phenomenon as well in the summer of 2020 as different states, tired of the lockdowns, acted as if the epidemic were over, even though, biologically speaking, it was not. It was wholly understandable that everyone was eager to leave the epidemic behind as quickly as possible. But the epidemiological reality did not submit to our desires. The pandemic was still claiming roughly a thousand lives per day, although Americans seemed inured to it. Many people, and not just self-interested politicians, seemed to believe the SARS-2 epidemic could end by fiat.
Last paragraph:
Microbes have shaped our evolutionary trajectory since the origin of our species. Epidemics have done so for many thousands of years. Like the myth of Apollo’s arrows, they have been a part of our story all along. We have outlived them before, using the biological and social tools at our disposal. Life will return to normal. Plagues always end. And, like plagues, hope is an enduring part of the human condition.
A must read. This is my preferred book reference on current pandemic.
Figure 16: The mortality impact of COVID-19 in the United States can be quantitatively compared to that of other modern epidemics.
09 de març 2023
Una de les fites més grans de la ciència: mRNA i les vacunes
La vacuna. La carrera para desarrollar una vacuna contra la COVID-19
Elegimos ir a la Luna. Crónica desde dentro de cómo se hizo posible lo imposible
The Messenger: Moderna, the Vaccine, and the Business Gamble That Changed the World
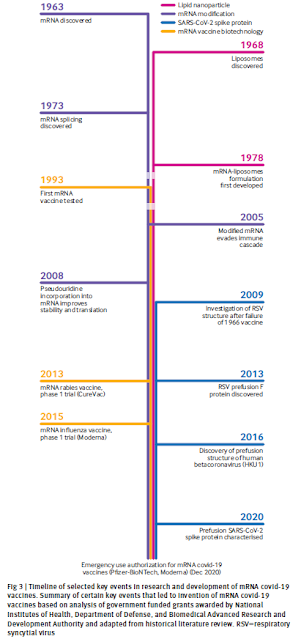
Just he acabat de llegir aquests tres llibres que fan referència a la vacuna BionTech-Pfizer i ModeRNA pel SARS-CoV-2. Primer va BionTech, per un motiu elemental són els que tenien el coneixement i el que va passar es que no van fer com a ModeRNA que alhora es van dedicar a la fabricació. Pfizer va ser capaç de posar-la al mercat en temps record. I va primer de tot BionTech perquè és la persistència en la recerca la que els ha portat a aquest resultat extraordinari en temps i efectivitat. Començant per comprendre els fonaments i després per encapsular l'mRNA que codifica la proteïna S en nanopartícules lipídiques i així crear anticossos neutralitzants al virus SARS-CoV-2.
Aquesta és una de les grans fites que ha assolit la ciència en un temps molt curt. És cert, però portaven més d'una dècada treballant-hi sense cap producte al mercat. I mentrestant uns inversors alemanys seguien apostant per ells.
El cas de ModeRNA és molt similar. Tenen un enfocament clavat en el potencial del mRNA i el desenvolupen en càncer, però no assoleixen cap producte al mercat després d'una dècada. A diferència de BionTech, el govern nordamericà va donar-los moltes subvencions.
Al darrera de BionTech i ModeRNA hi ha un personatge que surt a tots els llibres i és clau per l'èxit, Barney Graham. Des de l'Institut de Malalties Infeccioses nord-americà és capaç d'oferir-los guiatge i suport. Crec que ell sol es mereixeria un llibre.
Ara passada la pandèmia comença la lluita de les patents. ModeRNA reclama a BionTech perquè diuen que ha utilitzat coneixement que havien patentat abans. I ja hi som. El que hi ha en joc és molt, perquè el nombre de patents és elevat i el mRNA seria una via molt exitosa d'afrontar nous tractaments per càncer i moltes més malalties. Crec que haurien d'aprendre del que va passar amb els anticossos monoclonals, ho vaig explicar fa temps.
Tres llibres fonamentals i recomanables per comprendre què significa mRNA i com hem arribat on som, sans i estalvis (encara que no tots, gairebé 7 milions de morts per COVID), i alhora és moment d'un reconeixement als inversors que van apostar per la recerca a llarg termini i que va justament en contra dels resultats a curt que espera Wall Street.
Després de llegir aquests llibres pensava com tant poca gent ha aconseguit fer tant per la humanitat. Gent amb un talent immens, fruit d'un esforç i persistència continuada.
PD. El que he escrit sobre vacunes.
15 d’abril 2020
The viruses to come
If you want to read a story of ebola outbreak and its implications beyond it, this is the book you have to read. It may be translated into a screenplay of a film.
At the end it says:
A family of viruses called the morbilliviruses is regarded by some experts as a leading candidate for the emergence of a previously unknown Level 4 monster that travels in the air. If there was no vaccine or drug for it, and if it was highly infectious, and if it floated out of peoples mouths, the virus could go around the world in a few weeks, traveling inside people who are flying on airplanes and walking through airport terminals, breathing.Glups!
15 de desembre 2020
Atul Gawande on this pivotal moment
Atul Gawande on Taming the Coronavirus
Can a vaccine be distributed fairly? What will be the impact of a large number of people not taking it—as they say they won’t? Atul Gawande, a New Yorker staff writer who was recently appointed to President-elect Joe Biden’s covid-19 task force, walks David Remnick through some of the challenges of this pivotal moment
And in FT: "I do think that the fundamental disaster of the United States is tying where you get your healthcare to where you work,"
Agree
Podcast in The New Yorker radio:
09 d’abril 2020
Understanding COVID-19
COVID-19 and risks to the supply and quality of tests, drugs, and vaccines
Virtual health care in the era of COVID-19
Daily briefing: This is the state of COVID-19 vaccine development now
Disease Control, Civil Liberties, and Mass Testing — Calibrating Restrictions during the Covid-19 Pandemic
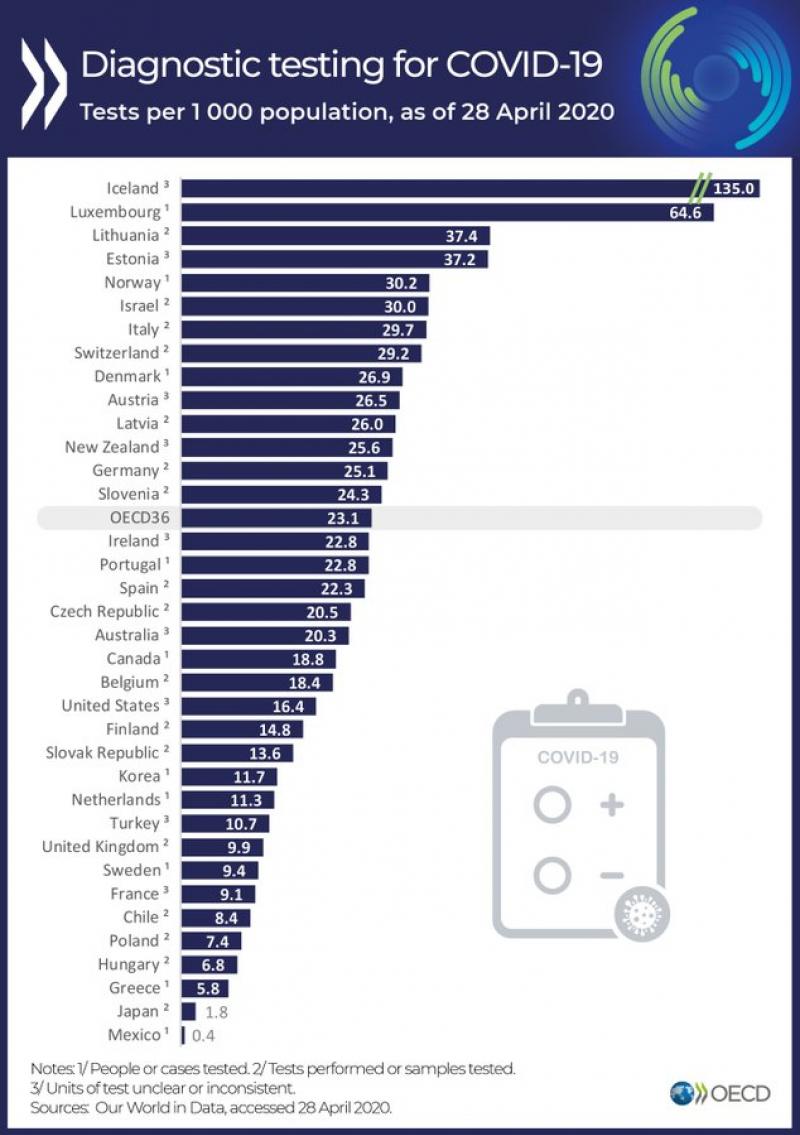
Thousands of coronavirus tests are going unused in US labs
Selected links on COVID-19.
From NEJM
Consider, for example, a policy in which people seeking to return to work, school, or social activities are asked to undergo baseline testing for infection and antibodies. Positive tests for infection would trigger self-isolation. Negative tests would certify freedom of movement for a defined period — say, 2 or 3 weeks — after which additional negative tests would renew the certification. If antibodies are determined to provide long-term protection against both reinfection and transmission — which is plausible but not yet established — a positive serologic test would warrant longer-term certification.And...if antibodies and infection are negative? What do you do? And... if this affects to 85% of population?. As is the case of Heinberg in Germany?
Aggregating test results at community and state levels would support a reliable disease-surveillance system. A testing regimen’s stringency could then be dialed up or down, depending on community prevalence of Covid-19. China is following a version of this approach by grading community risk on a four-tier, color-coded scale.
I would like to highlight the last one, how spply and demand for lab test doesn't match, in US and elsewhere...
29 de setembre 2021
The pandemic in US
Uncontrolled Spread. Why COVID-19 Crushed Us and How We Can Defeat the Next Pandemic
New book by Scott Gottlieb , former FDA comissioner
COVID revealed dangerous gaps in the US public health preparedness, medical infrastructure, and healthcare system. We lacked the public health capacity and resiliency we thought we had. In the most advanced healthcare system in the world, we ran out of medical masks. We had to retrofit anesthesia machines and turn them into respirators. We didn’t have enough swabs to collect samples from patients’ noses.
Our system was set up well to handle singular, technology-intensive, and complex problems like developing a novel vaccine or antibody drugs. We do this better than anyone. But it faltered when we were faced with more mundane problems like manufacturing those vaccines in bulk, deploying testing centers, or making nose swabs to collect respiratory samples. When we finally developed safe and effective therapeutics and vaccines that could treat or prevent infection, we couldn’t manufacture enough of them in time to supply the nation for the winter surge. We had to set up elaborate rationing schemes. Then, we were unable to establish an efficient distribution plan. Antibody drugs went unused because we couldn’t deliver them.
The virus made clear that we’ll need to fundamentally alter the way we approach all of these risks. If we don’t, our society will remain excessively vulnerable. For starters, we’ll have to lean much more on our intelligence agencies, and in a different fashion. International agreements alone haven’t provided us with the information we need about emerging threats. There’s little reason to believe they’ll perform much better in the future. The devastation caused by the pandemic proved that these risks, and our preparedness for them, is a matter of national security on par with other threats. We’re going to have to build the capacity to seek out the information we need to protect ourselves. Sometimes that will demand that we avail ourselves of the tools and tradecraft of our clandestine services. The challenge will be to maintain collaboration and multilateral efforts even as we turn more heavily toward intelligence services to guard against the risk of new contagions.
26 de setembre 2020
Viruses are among us
Viruses, Pandemics, and Immunity
A new book helps to explain our fight with infectious diseases. It splits it in two eras:
The first era of our eternal battle with infectious diseases ended with one of the major achievements of medicine, the vaccine against smallpox. We will tell the tale here of how this procedure, which ultimately eradicated the scourge of smallpox from the planet, was developed slowly by several cultures on different continents in an empirical way without any understanding of how or why it worked. In the second era we learned about the origins of infectious diseases and how to combat them.
And explains why we share our environment with viruses
Viruses are very simple ancient organisms that have probably existed since life began. For reasons that will become clear in the next section, viruses cannot reproduce on their own. They have to colonize bacteria, plants, and animals (including humans) in order to replicate and propagate their species. Therefore, viruses have specialized skills that let them invade other species and replicate inside them. When a virus invades the human body and replicates, it can damage our cells and tissues. The immune system, about which we will learn in the next chapter, tries to kill viruses that invade us to prevent and combat viral infections. This war between viruses and our immune system has raged since time immemorial.
And this is our current fight with SARS-CoV2. Highly recommended.
15 de març 2021
COVID epistemology
Why Does the Pandemic Seem to Be Hitting Some Countries Harder Than Others?
And there lies an epidemiological mystery. The usual trend of death from infectious diseases—malaria, typhoid, diphtheria, H.I.V.—follows a dismal pattern. Lower-income countries are hardest hit, with high-income countries the least affected. But if you look at the pattern of covid-19 deaths reported per capita—deaths, not infections—Belgium, Italy, Spain, the United States, and the United Kingdom are among the worst off.
This is the unfixed conundrum explained by Siddhartha Mukherjee in The New Yorker, And no clear answer, you may read the whole article to confirm it.
The covid-19 pandemic will teach us many lessons—about virological surveillance, immunology, vaccine development, and social policy, among other topics. One of the lessons concerns not just epidemiology but also epistemology: the theory of how we know what we know. Epidemiology isn’t physics. Human bodies are not Newtonian bodies. When it comes to a crisis that combines social and biological forces, we’ll do well to acknowledge the causal patchwork. What’s needed isn’t Ockham’s razor but Ockham’s quilt.
Above all, what’s needed is humility in the face of an intricately evolving body of evidence. The pandemic could well drift or shift into something that defies our best efforts to model and characterize it.
Great documentary, on Knoedle gallery fake art
14 de desembre 2021
The five essential healthcare suppliers
Taking access to the next level: mobilising five essential healthcare sectors
There are five groups that are crucial: Big Pharma, generic medicine manufacturers, vaccine manufacturers, diagnostics companies and medical gas companies.
In all cases, there are a few dominant players that have a big impact on healthcare
29 d’abril 2020
07 de març 2021
Vaccine access, now!
A compulsory licence allows a third party to produce a patented technology without the patent holder’s permission. Article 31 of the TRIPS Agreement allows all WTO States to issue compulsory licences subject to certain criteria.19 First, all cases are considered on their individual merits. Thus, a blanket compulsory licence for certain technologies, for example, medicines, is not possible. Second, prior attempts to negotiate a licence for the invention on reasonable terms with the patent holder must be evident. This requirement can be waived in ‘a national emergency or other circumstances of extreme urgency or in cases of public non-commercial use’ which would likely apply for COVID-19. Third, the scope/duration of the licence must be for the limited purpose it was authorised for. Fourth, the licence is non-exclusive so the patent holder can still enter into licensing agreements with others. Fifth, use of the licence is generally permitted predominantly for the supply of the domestic market of the State where the compulsory licence is granted. Finally, the patent holder must be paid ‘adequate renumeration’ for the compulsory licence.
So,
Crucially, it is only by starting a deeper conversation around the role of patent holders within the health context for COVID-19 and of the role of the public interest within patent law more generally that we can address and pre-empt some of the current obstacles posed by patents to equitable global access to healthcare. Given the significant health implications at stake it is vital that this conversation is informed by a global health and bioethics perspective
13 de juliol 2023
Una nova mesura de la morbiditat poblacional
En Randy Ellis ja abans de la pandèmia estava apuntant cap un nou sistema que permetés la mesura de la morbiditat amb dades diagnòstiques sense una classificació categòrica dels pacients. És a dir es tracta d'una evolució dels models que ell ha proposat des de fa anys junt amb Arlene Ash, els DCGs, i alhora una evolució del Clinical Classification Software.
L'objectiu:
Our objective was to create a clinically detailed, transparent, well-documented, nonproprietary classification system suitable for predicting diverse outcomes using ICD-10-CM diagnostic information and share a core set of predictive models that can be used on other data sets and populations.
Els tres tipus:
We created 3 types of DXIs. The primary or main effect DXIs, called DXI_1, focus on clinical dimensions in each diagnosis. Diagnoses were assigned up to 4 DXI_1s. In some cases, we created both broader and narrower DXI_1s that overlapped because we did not know a priori the level of detail preferred for prediction. We illustrate this approach below in our discussion of sepsis and hypertension in pregnancy DXI_1s.
The second group, DXI_2 modifiers, cut across DXI_1s. Some identify disease severity, such as “with complications,” “hemorrhage,” “secondary,” “bilateral,” and “with coma.” Others may be useful for disease monitoring, including flags for future research and epidemiological surveillance, such as sexually transmitted and vaccine-preventable infectious diseases. Certain diagnoses for external causes and factors influencing health status (whose codes begin with V-Z) were not assigned a DXI_1 and were instead only assigned DXI_2 modifiers.
Finally, DXI_3 scaled variables capture test results, disease severity, or clinically relevant distinctions not easily captured in binary DXI_1 categories. These include body mass index (BMI; calculated as weight in kilograms divided by height in meters squared), neonatal birth weight, neonatal gestational age, pregnancy trimester, low vision/blindness stages, coma scale measures, stroke scores, and duration of unconsciousness. As an example, the DXI_3 variable for BMI, calculated as weight in kilograms divided by height in meters squared, takes on values between 18.5 and 70, corresponding to ordered groups of BMI ranges. When comparing the DXI classification system to existing models, we included only main effects (DXI_1s) as predictors. This comparison cleanly demonstrates the value of the DXIs richer classification of diagnoses. Quantifying the additional value of using DXI_2 and DXI_3 items is left for future research.
Exemples:
La capacitat predictiva en despesa, aquí:
Si això és així, caldrà provar-ho ben aviat, amb 2929 variables explicatives assoleix una variació explicada del 51%.
El software per provar-lo en SAS aquí.
13 de març 2021
COVID-19 innovation response
The COVID-19 Innovation System
EIT Community COVID-19 Response
The COVID-19 innovation system represents a departure from business as usual. Considering the remarkable progress to date, especially on vaccine development, this raises the question of whether this model is useful only for crisis times, or whether biomedical innovation policy in “normal” times might productively incorporate some elements of the COVID-19 model as well.
The largest funding response has been from the US government. Roughly $14–$15 billion of the $4 trillion allocated to the COVID-19 response was for R&D for vaccines and treatments.8,9 Though this increased US federally funded biomedical R&D by about one-third (compared to previous NIH funding; see “NIH Data” in the online appendix),10 it is small compared with the potential value of these interventions for ameliorating or preventing the disease and securing a return to normalcy
18 de març 2020
Current coronavirus pandemic in context
Some months ago in the best books of FT 2019, I listed this one. and the summary is:
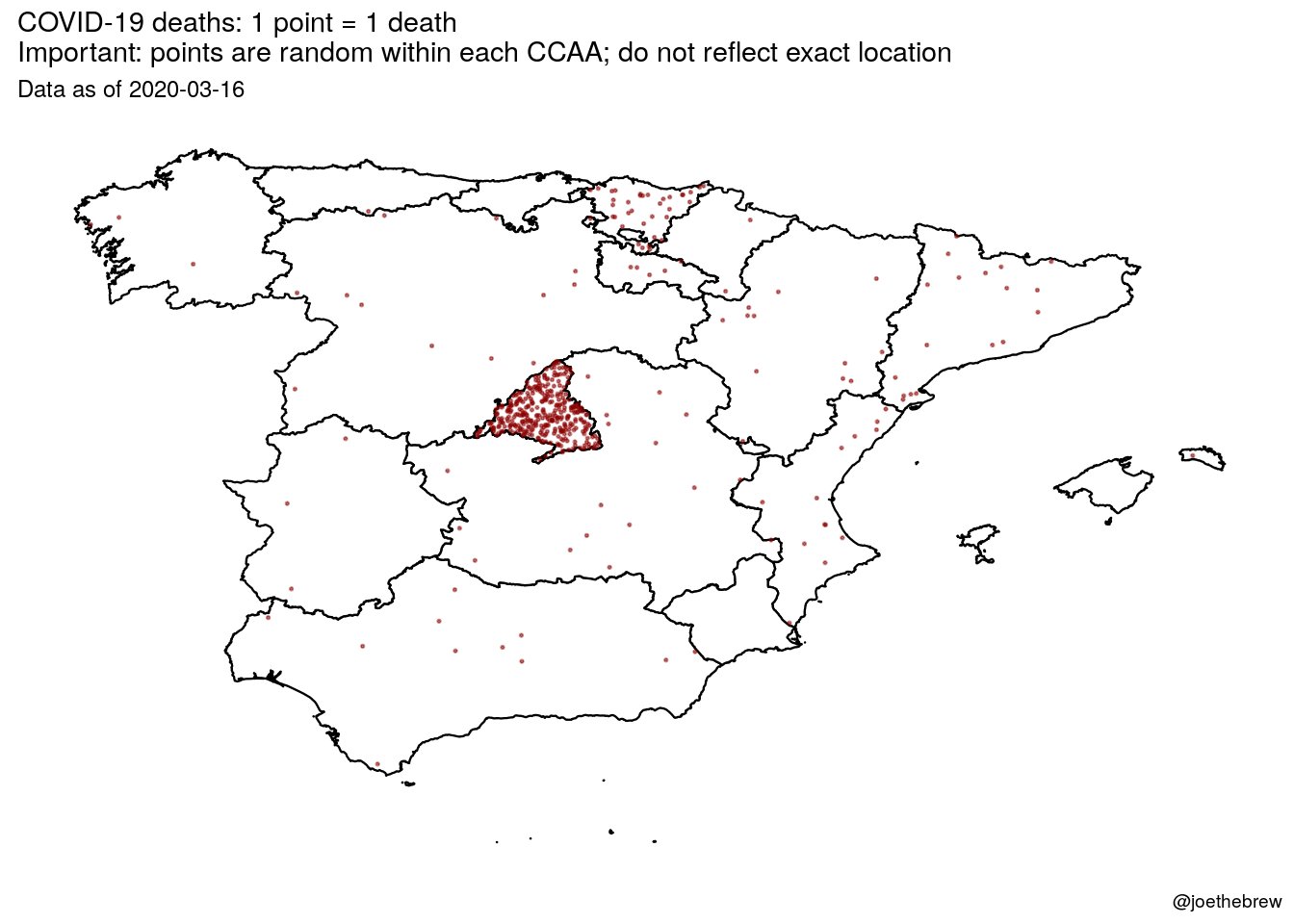
The Pandemic Century exposes the limits of science against nature, and how these crises are shaped by humans as much as microbes.This is exactly what is happening right now!!! Contagion is shaped also by politicians.
Just have a look at what's going on in Madrid. This is horrendous! And politicians don't want to close Madrid! And they have allowed to spread contagion outside. Somebody should say it louder. International health rules should prevail over spanish rulers.
Beyond politicians, there are experts.
Battered by their repeated failure to predict deadly outbreaks of infectious disease, even the experts have come to recognize the limits of medical prognostication. This is not only because microbes are highly mutable—that has been known since Pasteur’s time—but because we are continually lending them a helping a hand. Time and again, we assist microbes to occupy new ecological niches and spread to new places in ways that usually only become apparent after the event. And to judge by the recent run of pandemics and epidemics the process seems to be speeding up.
Reviewing the last hundred years of epidemic outbreaks, the only thing that is certain is that there will be new plagues and new pandemics. It is not a question of if, we are told, but when. Pestilences may be unpredictable but we should expect them to recur. However, what Camus could not have foreseen is that the attempt to anticipate disaster also creates new distortions and introduces new uncertainties. Twice this pandemic century, in 1976 and again in 2003, scientists thought the world was on the brink of a new influenza pandemic, only to realize that the outbreaks were false alarms and that the real danger lay elsewhere. Then in 2009 the WHO declared that the Mexican swine flu, a ressortment of two well-known H1N1 swine-lineage viruses that had circulated separately for over a decade, met the criterion of a pandemic virus, triggering the activation of global pandemic preparedness plans. On paper, this was the first pandemic of the twenty-first century and the first influenza pandemic in forty-one years. The fact that the swine flu was an H1N1, just like the Spanish flu, raised the prospect that this might be the Big One and that governments should expect a wave of illness and deaths similar to that in 1918–1919. But though the WHO’s declaration sparked widespread panic, the anticipated viral Armageddon never materialized. Instead, when it was realized that the Mexican swine flu was no more severe than a seasonal strain of flu, the WHO was accused of “faking” the pandemic for the benefit of vaccine manufacturers and other special interests. The result is what Susan Sontag calls “a permanent modern scenario: apocalypse looms . . . and it doesn’t occur.” As we look to the next one hundred years of infectious disease outbreaks, let us hope that is one prognostication that turns out to be true.
29 d’abril 2021
What you should know about the Covid-19 vaccines?
The Covid-19 Vaccine Guide. The Quest for Implementation of Safe and Effective Vaccinations
A book that explains all the details of one of the greatest achievements in medical research,
In the United States, in just over 11 months, two mRNA vaccines were developed and manufactured in parallel, tested in phase 1, 2, and the phase 3 large clinical trials, found to be safe and efficacious, and distributed initially in December 2020 to healthcare workers and residents of long-term care facilities, followed by those over 65 and with underlying medical conditions in January 2021. The story of that remarkable scientific and manufacturing accomplishment is described later in this chapter.
Why do these vaccines work? What is an immune correlate of protection? Vaccines are designed to induce a human immune response that prevents individual disease and may prevent or shorten individual infections. Much of the background for SARS-CoV-2 vaccines was initially based on the research on SARS-CoV infections, which in 2003 caused a global outbreak in 26 countries, the work on another novel coronavirus MERS, the long-term studies of other coronaviruses, and the work on other respiratory viruses such as respiratory syncytial virus (RSV).
In addition to individual protection, vaccines may also induce community or “herd” protection by decreasing transmission of the virus from one individual to another. We know that the two initial mRNA vaccines prevent illness with 94–95% efficacy in individuals. However, we do not yet know if they prevent infection or transmission.
10 de març 2023
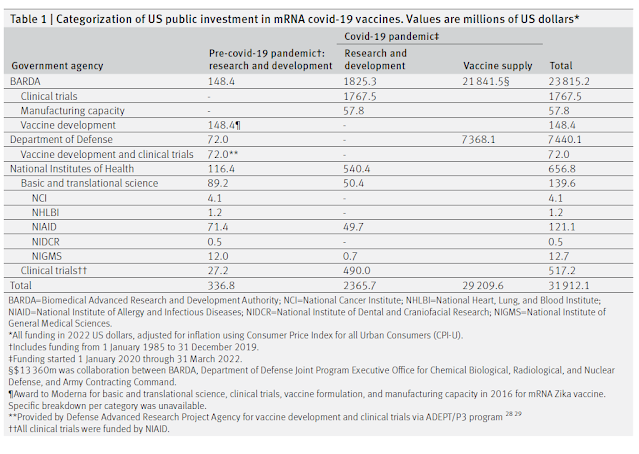
Quina va ser la inversió pública a la recerca de la vacuna mRNA per a covid?
US public investment in development of mRNA covid-19 vaccines: retrospective cohort study
Allò que observem i es veu reflectit als diaris no és pas necessàriament el que passa. Ho sabem. La dificultat es troba en esbrinar com la immediatesa de la informació perd peces importants a considerar per comprendre la realitat. L'exemple de la inversió pública en vacunes és molt clar. Hi va haver unes empreses que van fer accessible la vacuna a la població, però qui va invertir realment per arribar a aquest final?.
Al BMJ trobareu una resposta parcial, la part d'inversió pública nordamericana en R+D, que abans de la pandèmia va ser de 336,8 milions de $ i durant la pandèmia va ser de 2.365,7 milions de $, un total de 2.704,5 milions de $. Es tracta d'una xifra notable que ja s'havia recollit aproximadament en una publicació anterior de Richard Frank a Health Affairs. La taula adjunta explica els detalls de qui hi va contribuir i amb quin import:
The development of mRNA covid-19 vaccines during the pandemic was a monumental scientific success. This achievement was possible, in large part, because of significant US public investment in research and development during the preceding 35 years and record setting public contributions during the pandemic to accelerate and reduce the financial risk of vaccine development. The resulting mRNA vaccines have benefitted millions of people and saved millions of lives. The substantial role played by public funding should help to justify greater efforts by the US, Canadian, and German governments to assure equitable and affordable access to this lifesaving technology in the US and globally.