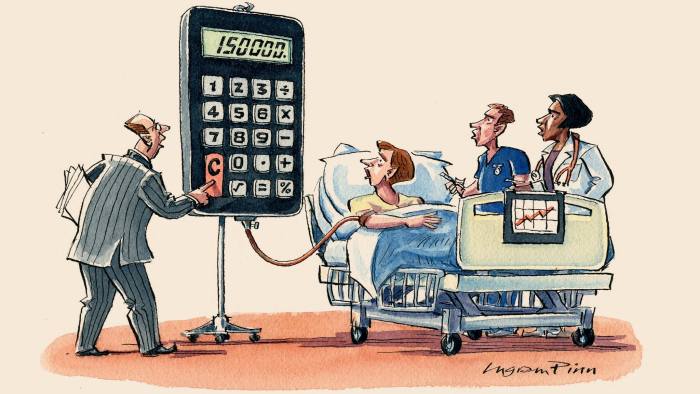
Nowadays, obesity prevention lies at the heart on any public health policy. If sugar sweetened beverages contribute decisively to obesity, then something should be done. What?. A recent PLOS article explains the options:
The main regulatory approaches are taxes, restrictions on the availability of SSBs in schools, restrictions on advertising and marketing, labeling requirements, and government procurement and benefits standards.On taxes:
Savvy regulatory design has tremendous potential. For example, there is growing evidence that taxes that are more salient to consumers, such as those included in a good’s posted price (rather than being levied at the register), are more likely to influence purchasing behaviorOn public procurement, a practical suggestion for immediate application:
Restrictions on which beverages may be purchased using government funds are a less visible form of regulation, but one with potential to change the consumption patterns of large numbers of people. Outside public schools, these standards are most germane in two areas: procurement standards for public institutions (e.g., government agencies, hospitals, and prisons) and restrictions on what recipients of government benefits for the indigent may buy with those funds.
The UK’s Government Buying Standards prohibit central government bodies from procuring SSBs larger than 330 ml and encourage the wider public sector to follow the guidelines. Massachusetts and many US counties and cities have adopted nutrition standards for government contracts, but most apply to a limited set of institutions, such as childcare facilities or youth centers.
PS. My former posts on the same topic.
PS. Article: The impact of sugar sweetened beverages on depression risk in adults.
PS. Report: Scenarios of Macro-economic Development for Catalonia on Horizon 2030
PS. Report: FBBVA Essential Public Services.
PS. Report: Chronicle of a premeditated offensive.