Elgar Encyclopedia of Healthcare Management
Una enciclopèdia amb aquest índex.1 Big data and artificial intelligence 2
2 Disruptive technology innovations 6
3 Genomics 8
4 Globalization 11
5 Medical tourism 13
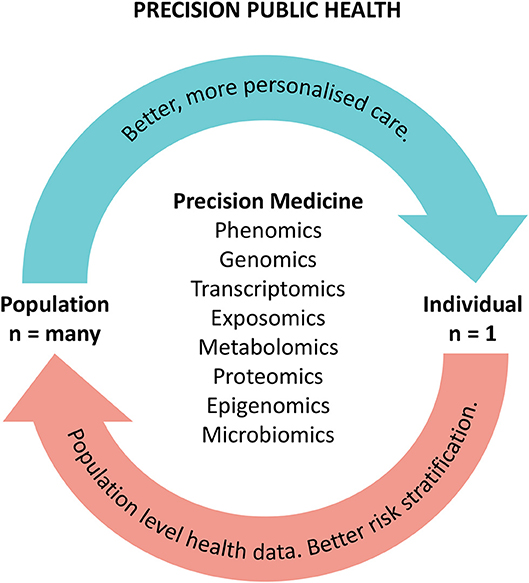
6 Precision medicine 16
7 Robotics 19
8 Beveridge model 22
9 Bismarck model 24
10 Market-driven model 26
PART III EVOLUTION OF THE PHARMA AND MEDTECH INDUSTRY
11 Market access 30
12 Digital therapeutics 33
13 Biotech 36
PART IV FOUNDATIONS OF HEALTH ECONOMICS
14 Baumol’s cost disease 40
15 Disease mongering 42
16 Moral hazard in health insurance 44
17 Quasi-markets 46
18 Supplier-induced demand 48
PART V FUNDING
19 Payment mechanisms 51
20 Sources of funding 55
21 Tariff vs price 57
PART VI HEALTH POLICY PRINCIPLES
22 Equality and equity 60
23 Universalism 62
24 Well-being 64
PART VII INVESTMENT ANALYSIS
25 Business planning of healthcare services 69
26 Sources of funding for investments 71
PART VIII LEVELS OF CARE
27 Acute, sub-acute and post-acute care 77
28 Chronic care 79
29 Home care and community care 83
30 Hospital 86
31 Long term care 91
32 Prevention 93
33 Screenings 97
34 Primary healthcare 101
35 Secondary vs tertiary vs quaternary care 104
PART IX NEW PARADIGMS
36 Access to healthcare 108
37 Co-production 110
38 Demedicalization 113
39 Evidence-based medicine 115
40 From compliance to concordance 119
41 Gender medicine 121
42 Global health 123
43 Health literacy 125
44 Initiative medicine 127
45 Integrated care 130
46 Population health management 133
47 Skill mix and task shifting in healthcare 136
48 Value-based vs
PART X PLAYERS
49 Boundaryless hospital 142
50 Community and country hospital 144
51 Intermediate and transitional care settings 147
52 Primary care center 150
53 Research hospital 152
54 Teaching hospital 154
PART XI TRENDS
55 Business models 157
56 Decentralization and devolution in healthcare 159
57 Multidisciplinarity and inter- professionality 161
58 Telemedicine 164
59 Vertical and horizontal integration (hub and spoke network) 168
PART XII BEHAVIOURS:
CHALLENGES TO LEADING HEALTH ORGANIZATIONS
60 Accountability 173
61 Accountable care plan and organization 174
62 Iatocracy, professional bureaucracy and corporatization 177
63 Political arena 180
64 Professional vs managerial culture 182
65 Professionalism 184
66 Stakeholder management 186
67 Teamwork 187
68 Turf wars 189
PART XIII PRACTICES
69 Change management 193
70 Disaster management 195
71 Leadership and leadership styles 199
PART XIV ROLES
72 Case manager 203
73 Clinical engineer 205
74 Clinical leader 208
75 Controller 211
76 Family and community nurse 215
77 General practitioner 218
78 Hospitalist 220
79 Medical director 223
80 Operations manager 225
81 Pharmacist 228
82 Quality and risk manager 233
PART XV TOOLS SYSTEM AND
PROCESS: DISEASE MANAGEMENT
83 Clinical governance 237
84 Guidelines and protocols in healthcare systems 239
PART XVI INNOVATION MANAGEMENT
85 Clinical trial 243
86 Health technology assessment 246
PART XVII OPERATIONS
87 Electronic clinical records 251
88 Patient flow logistics 253
89 Patient management 256
90 Supply chain 258
91 Techniques for process and organizations improvement: lean management in healthcare 261
PART XVIII ORGANIZATION
92 Clinical service lines 264
93 Converging trends in hospital transformation 267
94 Divisionalization, clinical directorates and Troika model in healthcare 271
95 Organizational culture 273
96 Organizational design and development for healthcare organizations 276
97 Patient-centered hospital and health organization 281
PART XIX PEOPLE
98 Clinical and professional engagement 285
99 Great Place to Work® 288
100 Magnet hospital 291
PART XX PERFORMANCE
101 Balanced scorecard in healthcare organizations 294
102 Budgeting (financial vs operational) 298
103 Customer satisfaction 301
104 DRG and case mix index 303
105 Length of stay 305
106 Performance measurement and management systems 307
107 PROMs and PREMs 310
108 Strategic control 313
PART XXI PLANNING
109 Strategic planning 318
110 Strategy making 320
PART XXII PROCUREMENT
111 Centralized procurement 324
112 Innovation procurement 327
113 Managed entry agreements (MEA) 330
114 Value-based procurement 333
PART XXIII QUALITY
115 Accreditation in healthcare 337
116 Audit 340
117 Quality management 343