Sick with “Shareholder Value”: US Pharma’s Financialized Business Model During the Pandemic
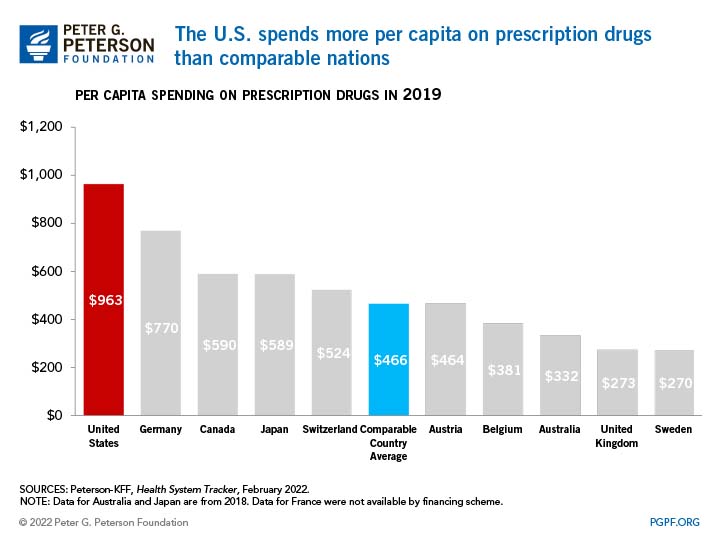
Als USA, la Inflation Reduction Act ha obert la caixa dels trons. La possibilitat que el govern pugui negociar els preus dels medicaments finançats públicament ha desesperat a la indústria que ha engegat una campanya de lobby inusual. Es tracta de protegir els preus alts perquè altrament no hi haurà innovació, això diuen. Però malgrat aquesta campanya, fa pocs dies el WP ja deia que no se n'han sortit i que estem propers a grans canvis, que es resumeixen en aquests 6:
1) Drug price negotiation
2) A cap on out-of-pocket spending
3) Lower prices for insulin
4) Free vaccines
5) Inflation penalty for drug manufacturers.
6) Extra help for the most vulnerable
El govern vol estalviar fins a 100.000 milions $ en aquests propers anys. I destacaria especialment, això de que si volen augmentar el preu més que la inflació (d'aquells medicaments ja en el mercat) hauran de fer descomptes al finançador públic. Dissuasió per tant de provocar preus excessius.
I aquí és on entra Wall Street que ho rebutja de dalt a baix i que ho veu com una amenaça al model de financialització que ha funcionat fins ara. Diuen que fins a 100 medicaments ja no arribaran al mercat. I aquesta amenaça no creïble no és certa perquè sabem això:
Data for the 474 corporations included in the S&P 500 Index in January 2022 and publicly traded from 2012 through 2021 reveal that these corporations distributed $5.7 trillion as share repurchases during the 2012-2021 fiscal years, representing 55 percent of net income, and $4.2 trillion as dividends, an additional 41 percent of net income.
Les recompres d'accions a la borsa per part de les companyies són un 13% superiors al que dediquen a la innovació.

As shown in Table 1, for the decade 2012-2021, distributions to shareholders by the 14 pharmaceutical companies that were among the 474 S&P 500 companies in the database represented 110 percent of net income,7 a larger proportion than the highly financialized 96 percent for all 474 companies. At 55 percent, the stock buybacks of the subset of pharmaceutical companies was the same proportion of net income as the 474 companies, but, at 54 percent versus 41 percent, pharmaceutical dividends as a proportion of net income far exceeded that of all the companies in the dataset. The 14 pharmaceutical companies accounted for 3.1 percent of the revenues of all 474 companies but 6.6 percent of the net income, 6.6 percent of the buybacks, and 8.8 percent of the dividends. The $747 billion that the pharmaceutical companies distributed to shareholders was 13 percent greater than the $660 billion that these corporations expended on research & development over the decade.
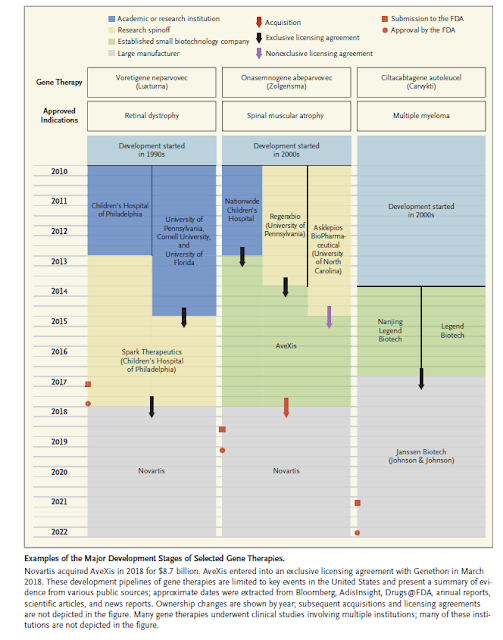
En aquest article de Lazonick hi trobareu molts més detalls sobre com ha canviat el model de negoci amb la biotecnologia. Si amb el model anterior el paper de la borsa era el típic de separació de propietat-control, en el nou les opas eren la forma de control per part de fons de capital-risc i després el paper del NASDAQ va oferir opcions d'entrada i sortida que abans no existien. L'article ho explica magníficament, no ho he vist enlloc més. La interacció de les recompres d'accions amb retribució escandalosa als directius de les companyies farmacèutiques esdevé una cosa mai vista a cap altra indústria.

Any 2021, el màxim directiu de Regeneron va ingressar 452 milions de $. No cal dir res més, tota la taula és una desmesura.
Què cal fer segons Lazonick?. El canvi en la regulació de preus és només el primer pas. Cal prohibir la recompra d'accions, deslligar el pagament dels directius dels valors de l'acció a borsa, posar representants dels accionistes al consell, reformar la fiscalitat de les empreses, encoratjar carreres professionals.
Molta feina per endavant si es vol capgirar la tendència de financialització dels medicaments que vivim. Altrament, un avís, tot el que als USA es disminueixi com ingressos, voldran que sigui compensat amb fons provinents d'altres països. Per tant cal estar alerta als moviments propers i avançar-se als esdeveniments.