Sickening. How Big Pharma Broke American Health Care and How We Can Repair It
20 de març 2022
11 de març 2022
10 de març 2022
Stop misuse of antibiotics
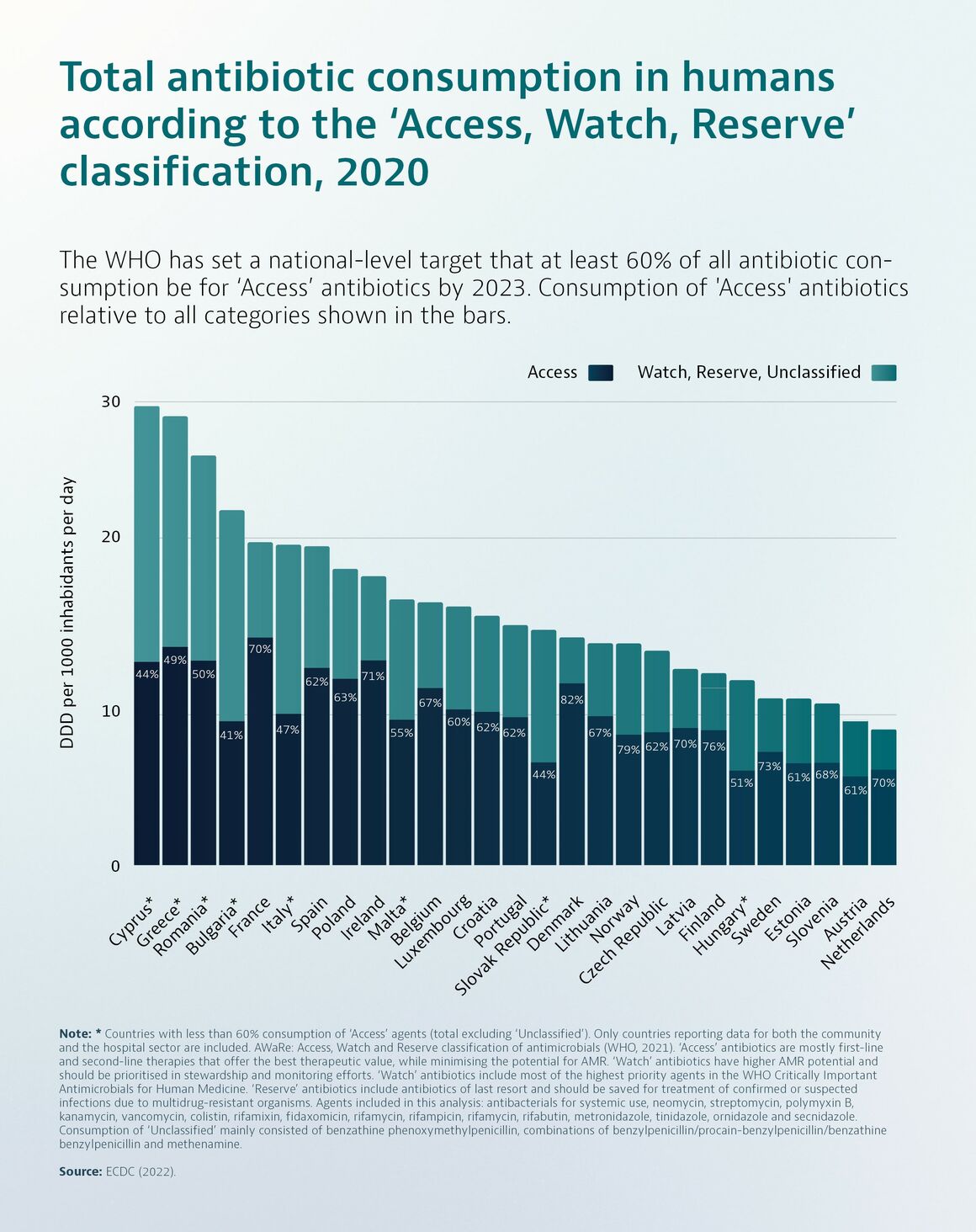
Antimicrobial Resistance in the EU/EEA: A One Health Response
Misuse of antibiotics is among the main drivers underpinning the development of antimicrobial resistance (AMR). Resistance to last-line antibiotics also compromises the effectiveness of life saving medical interventions such as intensive care, cancer treatment and organ transplantation.
Overall consumption of antibiotics in humans in the European Union/European Economic Area (EU/EEA) decreased by 23% between 2011 and 2020, especially during the Coronavirus Disease 2019 (COVID-19) pandemic (between 2019 and 2020, the mean total consumption of antibiotics dropped by almost 18%). However, relative use of broad-spectrum antibiotics has increased and significant variability across countries suggests that reductions are still possible.
Efforts to reduce unnecessary use of antibiotics in food-producing animals have resulted in a 43% decrease in use between 2011 and 2020 in 25 countries with consistent reporting.
Despite reductions in antibiotic consumption in both humans and food-producing animals, AMR in bacteria from humans in the EU/EEA has increased for many antibiotic-bacterium combinations since 2011. Particularly worrisome is the rise in resistance to critically important antibiotics used to treat common healthcare-associated infections.
While recent trends have been encouraging, resistance to commonly used antibiotics in bacteria from food-producing animals remains high (>20% to 50%) or very high (>50% to 70%), and there is significant regional variation across the EU/EEA region.
09 de març 2022
08 de març 2022
Public health genomics
From public health genomics to precision public health: a 20-year journey
Public health genomics focuses on effective and responsible translation of genomic science into population health benefits. We discuss the relationship of the field to the core public health functions and essential services, review its evidentiary foundation, and provide examples of current US public health priorities and applications
03 de març 2022
Value based health care (2)
Evaluación de resultados en salud: valor y sostenibilidad para el Sistema Nacional de Salud
Capítulo I. Evaluación de resultados en términos de salud: por qué, ¿cómo, cuándo y para qué?
Capítulo II. Resultados comunicados por los clínicos
Capítulo III. Resultados percibidos por los pacientes
Capítulo IV. Resultados en salud percibidos y comunicados por los observadores: ¿qué son y cómo se miden?
Capítulo V. ¿Cómo incorporar las medidas de resultados en salud a la evaluación económica?
Capítulo VI. Principales técnicas estadísticas y parámetros para medir resultados en salud
Capítulo VII. Metodología disponible para obtener resultados en salud en el mundo real
Capítulo VIII. Resultados en salud a evaluar en diferentes patologías: enfermedades infecciosas
Capítulo IX. Resultados en salud en la infección por VIH
Capítulo X. Resultados en salud en pacientes con hepatitis C crónica
Capítulo XI. Resultados en salud en reumatología
Capítulo XII. Resultados en salud en dermatología
Capítulo XIII. Resultados en salud en aparato digestivo: enfermedad inflamatoria intestinal e intestino irritable
Capítulo XIV. Resultados en salud en esclerosis múltiple
Capítulo XV. Beneficio clínico en oncología: una compleja pregunta
Capítulo XVI. Evaluación de resultados en salud: hematología
Capítulo XVII. Resultados en salud: patología cardiovascular
Capítulo XVIII. Resultados en salud a evaluar en enfermedades raras
Capítulo XIX. Investigación de resultados en salud en niños y adolescentes
01 de març 2022
23 de febrer 2022
22 de febrer 2022
Digital health futures
The governance of digital technologies in health and health care must be driven by public purpose, not private profit. Its primary goals should be to address the power asymmetries reinforced by digital transformations, increase public trust in the digital health ecosystem, and ensure that the opportunities offered by digital technologies and data are harnessed in support of the missions of public health and UHC. To achieve these goals, we propose four action areas that we consider game-changers for shaping health futures in a digital world.
First, we suggest that decision makers, health professionals, and researchers consider—and address— digital technologies as increasingly important determinants of health. Second, we emphasise the need to build a governance architecture that creates trust in digital health by enfranchising patients and vulnerable groups, ensuring health and digital rights, and regulating powerful players in the digital health ecosystem. Third, we call for a new approach to the collection and use of health data based on the concept of data solidarity, with the aim of simultaneously protecting individual rights, promoting the public good potential of such data, and building a culture of data justice and equity. Finally, we urge decision makers to invest in the enablers of digitally transformed health systems, a task that will require strong country ownership of digital health strategies and clear investment roadmaps that help prioritise those technologies that are most needed at different levels of digital health maturity.
21 de febrer 2022
Physician culture
Uncaring. HOW THE CULTURE OF MEDICINE KILLS DOCTORS & PATIENTS
The former CEO of Kaiser Permanente Medical Group shines a light on the unseen and often toxic culture of medicine (US and non-US).
Uncaring tells the story of a profession that is both triumphant and dangerously flawed, filled with people who aspire to help others, yet who sometimes act coldly, callously, and indifferently toward the pain of others. This book takes you inside the doctor’s world, revealing unique insights about their training, their daily practices, and the culture they share. It is a book about people striving for perfection and about the impossibility of achieving it. It sheds light on the norms, rules, and expectations of doctors, and shows how culture shapes their thoughts and beliefs. It deciphers their evolving language, symbols, and codes. It highlights what brings doctors together and what isolates them from their colleagues and patients. Finally, this book examines the elements of physician culture that need to be corrected, the ones that should be preserved, and how to accomplish both.
The exploration begins by diving into the meaning and relevance of “culture,” an abstract concept with myriad definitions and applications. Part One, “Diagnosing Physician Culture,” takes you behind medicine’s protective curtain. There you’ll be introduced to the rituals, icons, and beliefs physicians share.
Part Two, “The Physician’s Pain,” explores the complex interplay between the healthcare system and physician culture, showing how both have contributed to a burnout crisis that is now wreaking havoc on US doctors.
Part Three, “Helping or Harming Patients?,” focuses on the impact physician culture has on patients and the ways it contributes to the deterioration of our nation’s overall health.
Having detailed the reasons doctors feel overwhelmed, fatigued, and in perpetual conflict with the world around them, Part Four, “The Social Ladder,” looks at how changes in society are ratcheting up the discomfort physicians experience. Like the proverbial straw that breaks the camel’s back, each new societal influence seems, on the surface, relatively insignificant and completely manageable. But together, these changing norms are proving too much for physicians to handle.
Part Five, “The Evolution of Physician Culture,” offers patients, doctors, business leaders, and elected officials a difficult but necessary choice—one they will need to make in a world now socially, economically, and politically ravaged by the coronavirus. As the nation’s “new normal” takes shape, all the options involving the future of American medicine will be painful and risky. This section outlines those choices and the path toward making US healthcare, once again, the best in the world. Through the process, physician culture has an opportunity to change for the better.
By the end of this book, having observed physician culture under the proverbial microscope, you will be able to see in fine detail what has long remained invisible. You’ll better understand the doctors who provide your medical care and how you can protect yourself from their cultural shortcomings. Some of the stories in this book will inspire you and generate a deeper appreciation for the role doctors play in your life. Others will sadden you, opening your eyes to the many ways that physician culture compromises your health, harms our economy, and holds our country back.
20 de febrer 2022
Economics of pandemics (4)
The Economics of Pandemics. Exploring Globally Shared Experiences
Topics:
The COVID-19 Pandemic as a Globally Shared Experience: An Introduction
Pandemic Economics: Essential Features and Outstanding Questions
Pandemic Analysis I: Global Governance for a Global Pandemic?
Pandemic Analysis II: Governmental Actions During the Pandemic—Lockdown or No Lockdown?
Pandemic Analysis III: The Great Reset, People’s Uprisings, and Other Radical Change Proposals
Pandemic Analysis IV: Is the COVID-19 Pandemic a Doomsday Scenario for Climate Change?
Pandemic Analysis V: The Science and Economics of a Vaccine for Ending the Pandemic
The Economics of Pandemics as a Globally Shared Experience: A Theory
Some Yet Unresolved Questions and Mysteries About the COVID-19 Pandemic
18 de febrer 2022
17 de febrer 2022
The world is fat (2)
Can the Obesity Crisis Be Reversed?
From conclusions:
Ending the obesity epidemic will take both individual and collective action. Neither alone is sufficient. Individuals try to lose weight and keep it off, but the system is working against them. The route to population-wide weight loss will not be through trendy, unsustainable diets. It will be through widespread, appropriate, personalized, and comprehensive approaches.
The first action we all must take, no matter our size, is to educate ourselves about obesity—and you’ve been doing that by reading this book. People need to understand the structural, environmental, and genetic components of obesity. They need to see the ways in which systemic factors contribute to weight gain. The idea that obesity is a choice or a matter of willpower has been thoroughly disproved. The unfortunate fact that many people still believe this actively harms efforts to reduce obesity rates.
The government should first seek to change the public perception of obesity. Obesity is largely a result of structural forces, not just individual actions. A shared awareness of its origins could foster greater support for interventions that allow people to make healthier choices.
People and institutions need to work together to make healthy foods more accessible, affordable, appetizing, and convenient than unhealthy foods. Reversing the obesity crisis will require environments that promote physical activity and social movements that encourage people to get more exercise. We need to devote more resources to preventive efforts for all ages to improve our health.
To reverse the obesity crisis, we will need an all-hands-on-deck approach. Pharmacological advances, surgery, and other treatments should complement new policies, societal practices, and population-wide interventions that promote healthier diets and decrease food consumption. Improving the nation’s health may require implementing policies perceived as restricting personal freedoms that have long been granted to industries and individuals. But these policies will be essential to keeping the population healthy.
For individuals, the goal should be to reach and maintain your optimum weight, meaning the weight at which your body the optimal physical and mental health.
Outline of free ebook:
INTRODUCTION: Struggling with Obesity
CHAPTER 1: How Do People Gain Excess Weight?
CHAPTER 2: Why Are People Getting Heavier?
CHAPTER 3: What Are the Consequences of Obesity?
CHAPTER 4: What Are the Best Ways to Lose Weight?
CHAPTER 5: How to Reverse the Obesity Crisis