Physician Self-referral: Regulation by Exceptions
In 2002 a new agreement was published in internal medicine reviews on
Medical Professionalism in the New Millennium: A Physician Charter. Some years ago
I posted the same issue. Today, I would like to highlight three points again:
- Commitment to professional responsibilities. As members of a profession, physicians are expected to work collaboratively to maximize patient care, be respectful of one another, and participate in the processes of self-regulation, including remediation and discipline of members who have failed to meet professional standards. The profession should also define and organize the educational and standard-setting process for current and future members. Physicians have both individual and collective obligations to participate in these processes. These obligations include engaging in internal assessment and accepting external scrutiny of all aspects of their professional performance.
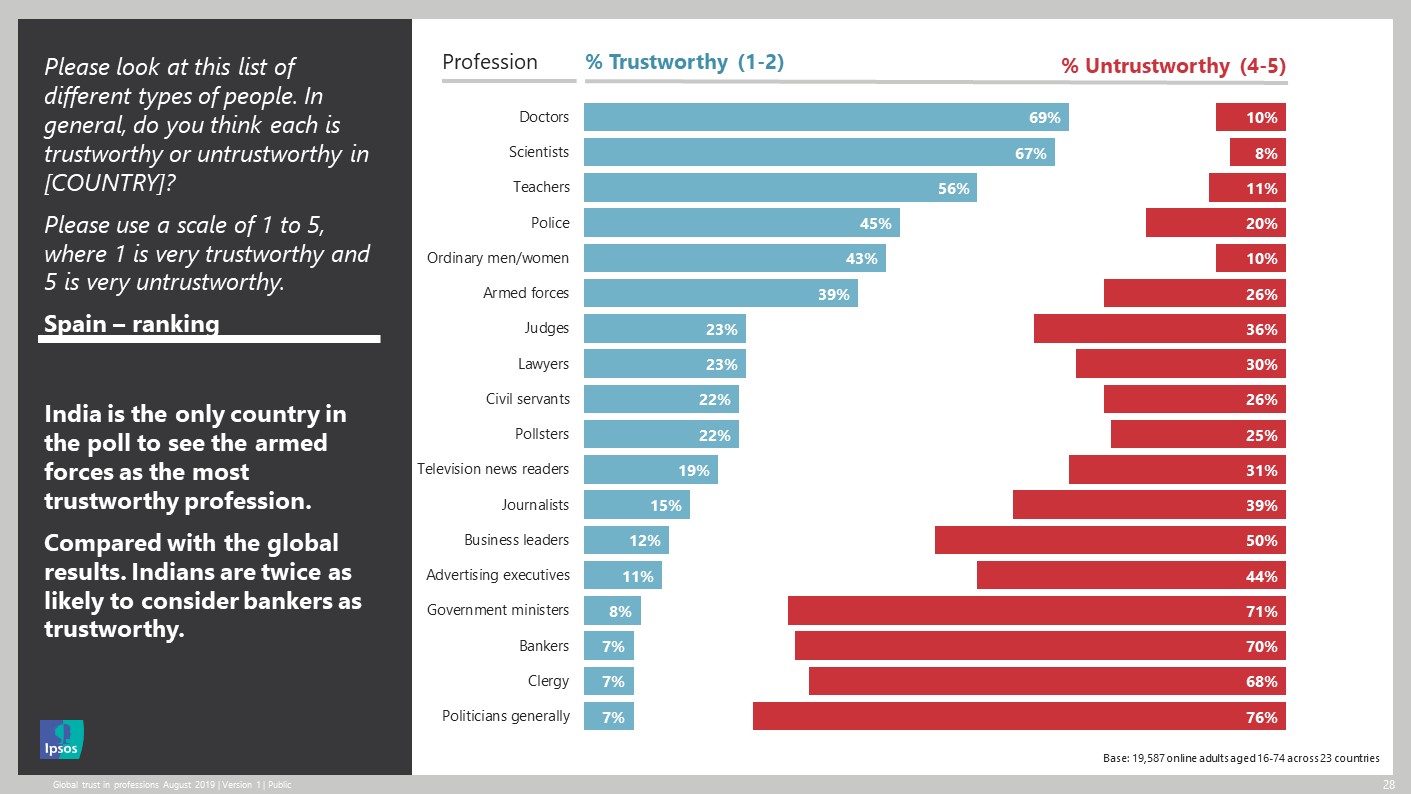
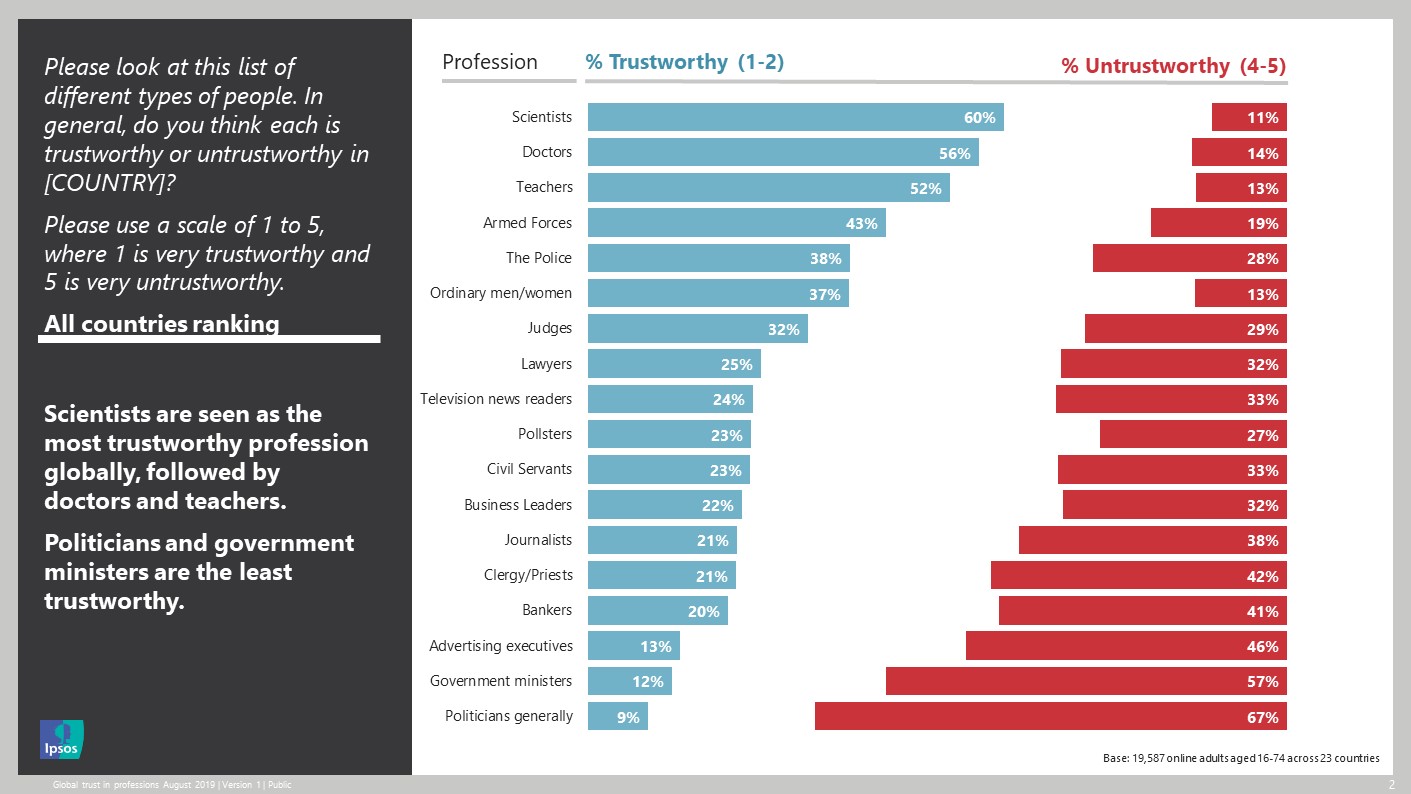
- Commitment to maintaining trust by managing conflicts of interest. Medical professionals and their organizations have many opportunities to compromise their professional responsibilities by pursuing private gain or personal advantage. Such compromises are especially threatening in the pursuit of personal or organizational interactions with for-profit industries, including medical equipment manufacturers, insurance companies, and pharmaceutical firms. Physicians have an obligation to recognize, disclose to the general public, and deal with conflicts of interest that arise in the course of their professional duties and activities. Relationships between industry and opinion leaders should be disclosed, especially when the latter determine the criteria for conducting and reporting clinical trials, writing editorials or therapeutic guidelines, or serving as editors of scientific journals
- Commitment to maintaining appropriate relations with patients. Given the inherent vulnerability and dependency of patients, certain relationships between physicians and patients must be avoided. In particular, physicians should never exploit patients for any sexual advantage, personal financial gain, or other private purpose.
After reading JAMA article on physician
self-referrals in US, definitely I have to say that this principles are far to be applied. The size of the resources coming from self-referrals is continously increasing despite the existing regulation for decades. The article puts a lot of expectations on changing the payment system, from fee-for-service towards value-based payments to curb the situation. I'm not so confident on this tool, because its implementation is far from optimal.
Anyway this is a difficult issue, and the same happens to
dual practice in general. Some weeks ago a new
resolution on how to handle conflicts of interest between public and private care was released. Two different concerns appear on my mind. The first is when any patient that decides to start a private treatment, then there is no option to go back to the public sector. He rejects explicitly public coverage. This statement may be appropriate for those patients on public waiting lists, but its application to other situations may be fuzzy. The second relates to information by the healthcare faciliy to patients about benefits and rights. I'm uncertain about how this can be applied without biases, without interference of physicians. My suggestion would be to use more transparent and centralised ways to inform patients through internet.
Unfortunately what I missed is precisely any regulation on physician self-referrals, the core of the problem. This affects publicly funded -in case of dual practice- and private care. Somebody should have a clear position on that. In my opinion, it should start by physicians associations. Self-regulation is a better starting point than any ban on this practice. As you may deduct easily, the general application of the former physician charter would solve this issue.