Apollo's Arrow. The Profound and Enduring Impact of Coronavirus on the Way We LiveFrom the book:
After its dramatic initial appearance, SARS-2 will ultimately become endemic; it will regularly circulate among us at some low, steady level. This is connected to the second kind of end, which we have already considered: herd immunity. Here, the pathogen is still around, but it has a much more difficult time reestablishing itself. This resembles a well-vaccinated population for any infectious disease; there are only occasional, small outbreaks among nonimmune people.
By 2022 or so, we will reach this outcome naturally or via vaccination. Of course, if we do rapidly develop and distribute a safe and effective vaccine, we could reach herd immunity with fewer deaths. Based on the fundamental R0 of SARS-2, as we saw in chapter 2, up to an estimated 60 to 67 percent of the population could be affected (or roughly two hundred million people in the United States). The necessary percentage could be lower, closer to 40 to 50 percent, given that social network structure means that different people spread the virus to different extents (as we also saw in chapter 2); or it could be higher, if the epidemic moves extremely fast and we overshoot the level required for herd immunity. Whatever the exact percentage, as a pathogen spreads, some people will die and others will recover and become immune, so eventually the virus will run out of places to go. This is the ordinary, natural way that, biologically speaking, epidemics end.
This is what we mean when we say that a pathogen is under control. But sometimes, plagues are so devastating that a society never recovers. It’s very important to emphasize that, as bad as COVID-19 is, it’s not remotely as bad as epidemics of bubonic plague, cholera, or smallpox that have killed much larger fractions of the population and that have had much larger and longer-lasting effects. Those types of plagues are even associated with the iconography of the Four Horsemen of the Apocalypse, Pestilence riding side by side with War, Famine, and Death. Those epidemics vindicated the adage that “too few of the living were left to bury the dead.”
N. Christakis says at the begining of the book
The god Apollo, for example, was both a healer and the bringer of disease. During the Trojan War, with his silver bow and quiver of arrows, he rained a plague down on the Greeks to punish them for kidnapping and enslaving Chryseis, the daughter of one of his favored priests.
I found myself thinking again about Apollo and his vengeance as I contemplated our own twenty-first-century barrage more than three thousand years after the events described in The Iliad. It seemed to me that the novel coronavirus was a threat that was both wholly new and deeply ancient. This catastrophe called on us to confront our adversary in a modern way while also relying on wisdom from the past.
Excerpts from the last chapter, How plagues end:
The pathogens evolve to respond to us, but we, at a slower pace, also evolve to respond to them. Infectious diseases have been a part of our evolutionary history for so long that they have left a mark on our genes. For instance, humans have evolved genetic changes that have proven useful in coping with malaria beginning over one hundred thousand years ago, tuberculosis over nine thousand years ago, cholera and bubonic plague over six thousand years ago, and smallpox over three thousand years ago.36
Infectious pathogens (even if nonepidemic) have arguably been a crucial selective pressure throughout the evolution of our species.37 The primary killers of human beings across evolutionary time are other human beings. Humans do not have any natural predators that substantially affect survival.38 Except for our microscopic enemies.
The SARS-2 virus is a lot less lethal to people of reproductive age and can be combated with the lifesaving tools of modern medicine, so the impact on human evolution is surely going to be minimal. But, at least in theory, another way epidemics end is that hosts evolve to be resistant. And in fact, we may already have naturally occurring genetic variation in our species that affects the severity of COVID-19 in different populations, which would lay the groundwork for such evolution. Over generations, this can result in changes to the genetic makeup of the afflicted populations.
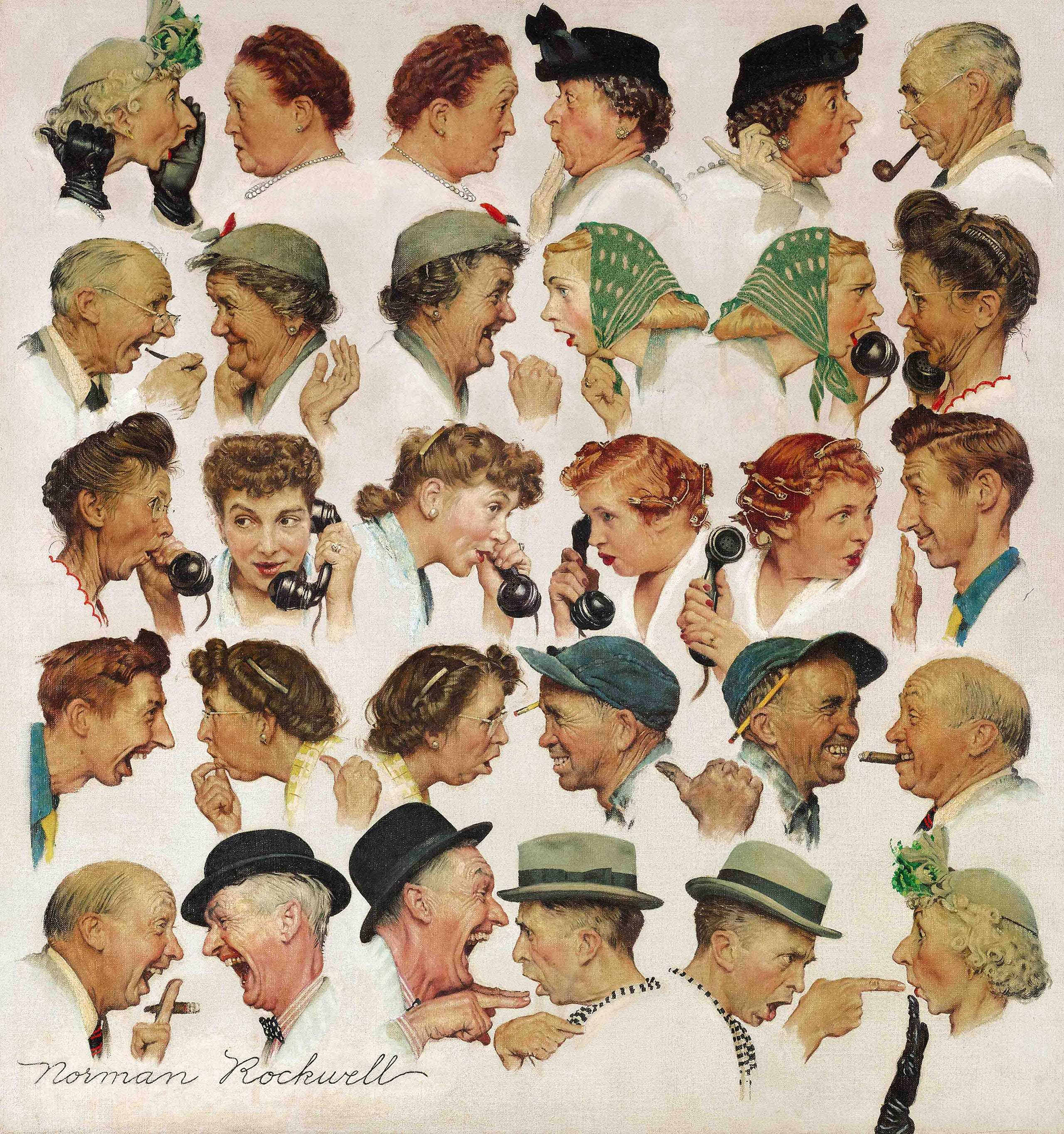
This social construction of COVID-19 means that the end of the pandemic can also be socially defined. In other words, plagues can end when everyone believes they are over or when everyone is simply willing to tolerate more risk and live in a new way. If everyone willingly risks infection and resumes a semblance of normal life (or, implausibly, if everyone decides to employ physical distancing forever), then the epidemic can be said to have ended, even if the virus is still circulating. We got a glimpse of this phenomenon as well in the summer of 2020 as different states, tired of the lockdowns, acted as if the epidemic were over, even though, biologically speaking, it was not. It was wholly understandable that everyone was eager to leave the epidemic behind as quickly as possible. But the epidemiological reality did not submit to our desires. The pandemic was still claiming roughly a thousand lives per day, although Americans seemed inured to it. Many people, and not just self-interested politicians, seemed to believe the SARS-2 epidemic could end by fiat.
Last paragraph:
Microbes have shaped our evolutionary trajectory since the origin of our species. Epidemics have done so for many thousands of years. Like the myth of Apollo’s arrows, they have been a part of our story all along. We have outlived them before, using the biological and social tools at our disposal. Life will return to normal. Plagues always end. And, like plagues, hope is an enduring part of the human condition.
A must read. This is my preferred book reference on current pandemic.
Figure 16: The mortality impact of COVID-19 in the United States can be quantitatively compared to that of other modern epidemics.