Some months ago, Mckinsey released a guide to AI for executives. It says:
Deep learning is a type of machine learning that can process a wider range of data resources, requires less data preprocessing by humans, and can often produce more accurate results than traditional machine-learning approaches (although it requires a larger amount of data to do so). In deep learning, interconnected layers of software-based calculators known as “neurons” form a neural network. The network can ingest vast amounts of input data and process them through multiple layers that learn increasingly complex features of the data at each layer. The network can then make a determination about the data, learn if its determination is correct, and use what it has learned to make determinations about new data. For example, once it learns what an object looks like, it can recognize the object in a new image.Now Nature publishes a helpful review article on deep learning in healthcare.
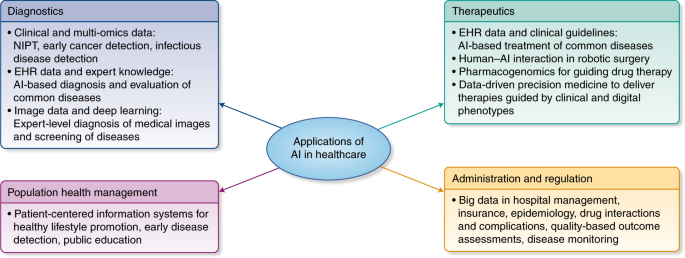
Some of the greatest successes of deep learning have been in the field of computer vision (CV). CV focuses on image and video understanding, and deals with tasks such as object classification, detection, and segmentation—which are useful in determining whether a patient’s radiograph contains malignant tumorsThe next step is speech and text. Some advances are already available. Basically, Tensorflow by Google is feeding the beast.
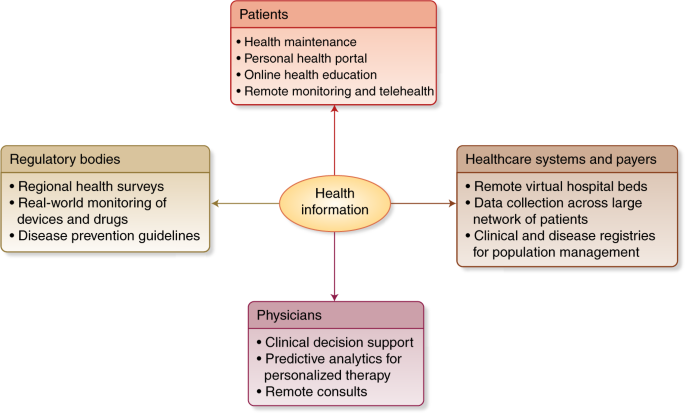
PS. WHO and the classification of digital health interventions 1.0
PS. And the book to read: