Finally the government has decided to organise genetic counseling and testing. A recent instruction determines who does what. As you may remember I've said several times that government was on permanent holiday on this issue.
In this new instruction, at least two issues are forgotten: the tests that are covered, and the proliferation of sequencing instruments outside the lab. These are not minor issues.
Somebody should decide asap wether a test it is worth to be prescribed. Right now, there are no explicit constraints under the current instruction. And DNA sequencing instruments may be found in many departments under the consideration of research. If there is no clear split between research and care, I can imagine a close future with many messy labs within any hospital. Concentration of knowledge and specialisation provides wider guarantees for quality. Unless there is any mentorship program by clinical laboratories, things will go down the wrong path. Today I'm more worried than yesterday, unless these two issues are fixed.
29 de juny 2015
17 de juny 2015
Changing health behavior (once again)
World Development Report 2015: Mind, Society, and Behavior
Understanding human behavior is one of the main scientific endevours of our current times. As I have explained before, psychology, economics and neurosciences are making great progress in the last decades. Now the annual report by the World Bank puts all this stuff in one publication:
Understanding human behavior is one of the main scientific endevours of our current times. As I have explained before, psychology, economics and neurosciences are making great progress in the last decades. Now the annual report by the World Bank puts all this stuff in one publication:
Three principles stand out as providing the direction for new approaches to understanding behavior and designing and implementing development policy. First, people make most judgments and most choices automatically, not deliberatively: we call this “thinking automatically.” Second, how people act and think often depends on what others around them do and think: we call this “thinking socially.” Third, individuals in a given society share a common perspective on making sense of the world around them and understanding themselves: we call this “thinking with mental models".In chapter 8 you'll find the application to health issues. A clear warning:
Telling people that there is a way to improve their health is rarely sufficient to change behavior. In general, successful health promotion campaigns engage people emotionally and activate or change social norms as much as they provide information. The message disseminated should be that others will support you or even applaud you if you do it, not just that something is good for you. Successful campaigns address many or most of the following: information, performance, problem solving, social support, materials, and media . A campaign should tell people that a behavior will improve their health (information), demonstrate and model the behavior (performance), reduce barriers to its adoption (problem solving), create a system for supporting people who choose to adopt it (social support), provide the materials necessary to begin adoption (materials), and provide a background of support through in-person, print, radio, television, and other approaches (media).As you may imagine, this is much more difficult than simply giving information. This is precisely the greatest challenge.
16 de juny 2015
Health across borders
Let's think of two countries artificially separated by political borders. Both have the same income per capita (~27,700 €) and belong to the EU. The first spends 11.1 % of GDP on health (5,513€ per capita, 77.7% public funding), while the second only 8% (3,898€ per capita, 65.8% públic funding).
Both countries have roughly the same life expectancy at birth. Healthy life expectancy at 65 is better in the country that spends less. The number of visits and hospitalizations is also less. Physicians are also paid less, 18% less in general practitioners income, up to 40% in specialists income.
There is only one border between them, an artificial border created by a treaty to end a war that lasted 30 years. This is the case of part of France and Catalonia. While the first can decide over the size of resources devoted to health, the second has no role on it, by now.
PS. Today at COMB, French health reform. I'll be there. #sanitatfrança
Both countries have roughly the same life expectancy at birth. Healthy life expectancy at 65 is better in the country that spends less. The number of visits and hospitalizations is also less. Physicians are also paid less, 18% less in general practitioners income, up to 40% in specialists income.
There is only one border between them, an artificial border created by a treaty to end a war that lasted 30 years. This is the case of part of France and Catalonia. While the first can decide over the size of resources devoted to health, the second has no role on it, by now.
PS. Today at COMB, French health reform. I'll be there. #sanitatfrança
15 de juny 2015
The value of vaccination
Valuing vaccination
A PNAS article sets a broader perspective on valuing vaccines. It is of interest in light of current difteria case. My position is clear, no doubt about mandatory vaccination if its cost-effectiveness is proven.
Suggestions from the article:
Framework of vaccination benefits
A PNAS article sets a broader perspective on valuing vaccines. It is of interest in light of current difteria case. My position is clear, no doubt about mandatory vaccination if its cost-effectiveness is proven.
Suggestions from the article:
Three general recommendations flow from our arguments and related synthesis of existing evidence on broad benefits of vaccination. First, many economic evaluation studies of vaccinations should be redone to capture the full benefits generated by the vaccination in question. Second, the evidence to date on the full value of vaccination has been focused on measuring the total social benefits generated. It would also be useful to explore the distribution of vaccination’s benefits among different possible beneficiaries. Third, the primary empirical evidence on broad vaccination benefits will need to be considerably expanded and improved
Framework of vaccination benefits
| Perspective | Benefit categories | Definition | |
| Broad | Narrow | Health care cost savings | Savings of medical expenditures because vaccination prevents illness episodes |
| Care-related productivity gains | Savings of patient’s and caretaker’s productive time because vaccination avoids the need for care and convalescence | ||
| Outcome-related productivity gains | Increased productivity because vaccination improves physical or mental health | ||
| Behavior-related productivity gains | Vaccination improves health and survival, and may thereby change individual behavior, for example by lowering fertility or increasing investment in education | ||
| Community health externalities | Improved outcomes in unvaccinated community members, e.g., through herd effects or reduction in the rate at which resistance to antibiotics develops | ||
| Community economic externalities | Higher vaccination rates can affect macroeconomic performance and social and political stability | ||
| Risk reduction gains | Gains in welfare because uncertainty in future outcomes is reduced | ||
| Health gains | Utilitarian value of reductions in morbidity and mortality above and beyond their instrumental value for productivity and earnings | ||
12 de juny 2015
Reviewing the residency system
Let Me Heal. The Opportunity to Preserve Excellence in American Medicine
We usually emphasize the level of resources when we assess the results of our health system. Institutions matter, we already know that. And if there is one key success factor in our healthcare is the physician's residency program. Training of the physicians under "real" conditions has allowed substantial improvements in health outcomes and the progress of medicine that are difficult to measure specifically. In a new book, Ludmerer provides an excellent review of what it represents to US healthcare:
PS. Must see. Documentary: Big Data, citizens under scrutiny.
We usually emphasize the level of resources when we assess the results of our health system. Institutions matter, we already know that. And if there is one key success factor in our healthcare is the physician's residency program. Training of the physicians under "real" conditions has allowed substantial improvements in health outcomes and the progress of medicine that are difficult to measure specifically. In a new book, Ludmerer provides an excellent review of what it represents to US healthcare:
At the core of the residency system are fundamental educational principles: the assumption of responsibility by residents in patient management, and the importance of providing residents sufficient time to reflect and pursue subjects in depth. Also at the core are the moral principles of residency training: thoroughness, attention to detail, and learning that the needs of patients should come firstAnd considers that
The current turmoil in health care delivery offers the profession and public the opportunity to redesign medical education and practice in ways that more fully serve the needs of patients, present and future. The opportunity is there to envision medical education and practice as they should be, not as they are, and to work toward achieving that end. Such opportunities are to be treasured, not feared. The country will always need good doctors, and the medical profession has little to fear in the changes ahead as long as it remembers that it exists to serve, that the needs of patients come before its own, and that it always must be thinking of improving the future as well as caring for the present.This call for a redesign of medical education and practice is a real need in our environment. The confusion between the role of "student" and "employee" is increasing and there is no effort to clarify it.The number of physicians in the program is determined without any clear estimation of demand and rules. A total mess. That's why I consider that we should rethink it from its foundations.
PS. Must see. Documentary: Big Data, citizens under scrutiny.
09 de juny 2015
Integrated care and population health
Population health Systems: Going beyond integrated care
In this blog I have mentioned several times the works by Kindig on population health. If integrated care makes sense, it is because it improves population health. Otherwise we should talk about diferent things.
A new report by the King's Fund sheds some light on several experiences of integrated care. It's worth reading, because you'll see that there is not only one way to achieve the final goal, and the tool -better coordination- has to be suited to the specific setting.
The "recipe":
In this blog I have mentioned several times the works by Kindig on population health. If integrated care makes sense, it is because it improves population health. Otherwise we should talk about diferent things.
A new report by the King's Fund sheds some light on several experiences of integrated care. It's worth reading, because you'll see that there is not only one way to achieve the final goal, and the tool -better coordination- has to be suited to the specific setting.
The "recipe":
At a practical level, developing a population health systems perspective requires the following elements as a minimum:
• pooling of data about the population served to identify challenges and needs
• segmentation of the population to enable interventions and support to be targeted appropriately
• pooling of budgets to enable resources to be used flexibly to meet population health needs, at least between health and social care but potentially going much further
• place-based leadership, drawing on skills from different agencies and sectors based on a common vision and strategy
• shared goals for improving health and tackling inequalities based on an analysis of needs and linked to evidence-based interventions
• effective engagement of communities and their assets through third sector organisations and civil society in its different manifestations
• paying for outcomes that require collaboration between different agencies in order to incentivise joint working on population health.
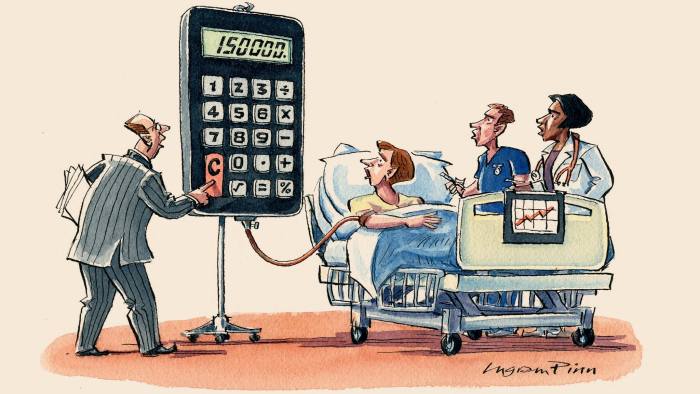
FT on cancer drugs pricing
08 de juny 2015
Being aware of what's going on in marijuana market
Waiting for the opportune moment: the tobacco industry and marijuana legalization
Is it possible to prevent another public health catastrophe similar to tobacco use?. This is the question posed by a recent article in Milbank Quarterly related to marijuana legalization. They explain with complete details how:
Is it possible to prevent another public health catastrophe similar to tobacco use?. This is the question posed by a recent article in Milbank Quarterly related to marijuana legalization. They explain with complete details how:
Since at least the 1970s, tobacco companies have been interested in marijuana and marijuana legalization as both a potential and a rival product. As public opinion shifted and governments began relaxing laws pertaining to marijuana criminalization, the tobacco companies modified their corporate planning strategies to prepare for future consumer demand.And their conclusion is clear:
Policymakers and public health advocates must be aware that the tobacco industry or comparable multinational organizations (eg, food and beverage industries) are prepared to enter the marijuana market with the intention of increasing its already widespread use. In order to prevent domination of the market by companies seeking to maximize market size and profits, policymakers should learn from their successes and failures in regulating tobacco.If this is so, why does nobody care about it?. Why aren't health politicians taking decisions in the right direction?. I strongly suggest them reading this article based on the documents of the tobacco industry and act accordingly.
05 de juny 2015
What's still wrong in economics (and health economics) research
Some weeks ago I was posting on "Evidence-based economics going mainstream" , in fact the title was only taken from the book by Thaler and it is strictly a desideratum. Unfortunately what we are used every week in the university seminars is more related to Chicago style economics: Optimization +Equilibrium = Economics.
The struggle to bring academic discipline back down to earth is an unfinished business. Let's take for example this paper: Can Health Insurance Competition Work? Evidence from Medicare Advantage. The author achieves this conclusion:
Improving health is the goal, and nobody can answer to this question with this methodologic approaches. Understanding the bounded rationality, heuristics and biases of individuals is fundamental to assess any policy. As Thaler says in his book:
PS. It's not a surprise that they have forgotten a key paper on the topic by R. Frank.
PS. Must see:
The exhibition Barcelona Haggadot reunites for the first time in more than six centuries an extensive selection of these splendid works of the Catalan Gothic period that were dispersed around the world when the Jews were expelled.
Barcelona, the seat of a monarchy and a hub of Mediterranean trade, had an urban ethos that was receptive to the most innovative artistic influences in the opening decades of the 14th century. At this juncture in the Gothic era, the city’s workshops constituted a highly active centre for the production of Haggadot, manuscripts that contain the ritual of the Passover meal, which were commissioned by families living in the Call (Jewish quarter) in Barcelona and in other Jewish communities. Jews and Christians alike worked on Haggadot and shared the same style and iconographic models.
PS. Victor Grifols has recently deceased. This obituary explains clearly his commitment with health, ethics and business. RIP
The struggle to bring academic discipline back down to earth is an unfinished business. Let's take for example this paper: Can Health Insurance Competition Work? Evidence from Medicare Advantage. The author achieves this conclusion:
We estimate that private plans have costs around 12% below fee-for-service costs, and generate around $50 in surplus on average per enrollee-month, after accounting for the disutility due to enrollees having more limited choice of providers. Taxpayers provide a large additional subsidy, and insurers capture most of the private gains.Is this a conclusion?. What are the gains? Monetary gains? Does it make any sense to compare an outdated system like fee-for service with another outdated one such as "managed competition"?
Improving health is the goal, and nobody can answer to this question with this methodologic approaches. Understanding the bounded rationality, heuristics and biases of individuals is fundamental to assess any policy. As Thaler says in his book:
Moreover, much of what economists do is to collect and analyze data about how markets work, work that is largely done with great care and statistical expertise, and importantly, most of this research does not depend on the assumption that people optimize. Two research tools that have emerged over the past twenty-five years have greatly expanded economists’ repertoire for learning about the world. The first is the use of randomized control trial experiments, long used in other scientific fields such as medicine. The typical study investigates what happens when some people receive some “treatment” of interest. The second approach is to use either naturally occurring experiments (such as when some people are enrolled in a program and others are not) or clever econometrics techniques that manage to detect the impact of treatments even though no one deliberately designed the situation for that purpose. These new tools have spawned studies on a wide variety of important questions for society.There is a long way forward in economic (and health economics) research.
PS. It's not a surprise that they have forgotten a key paper on the topic by R. Frank.
PS. Must see:
The exhibition Barcelona Haggadot reunites for the first time in more than six centuries an extensive selection of these splendid works of the Catalan Gothic period that were dispersed around the world when the Jews were expelled.
Barcelona, the seat of a monarchy and a hub of Mediterranean trade, had an urban ethos that was receptive to the most innovative artistic influences in the opening decades of the 14th century. At this juncture in the Gothic era, the city’s workshops constituted a highly active centre for the production of Haggadot, manuscripts that contain the ritual of the Passover meal, which were commissioned by families living in the Call (Jewish quarter) in Barcelona and in other Jewish communities. Jews and Christians alike worked on Haggadot and shared the same style and iconographic models.
PS. Victor Grifols has recently deceased. This obituary explains clearly his commitment with health, ethics and business. RIP
04 de juny 2015
Alcohol use and abuse
Tackling Harmful Alcohol Use
Tha last OECD report is focused on health impact of alcohol and what should we do to avoid harmful effects. Key findings are the following ones:
Tha last OECD report is focused on health impact of alcohol and what should we do to avoid harmful effects. Key findings are the following ones:
- Alcohol use has both beneficial and detrimental effects on the health of individualdrinkers. At the population level, the latter outweigh the former in all countries.
- The risk of death for young male adults and young and middle-aged women increasessteadily with alcohol consumption, with no beneficial effects overall, but with relatively
- Approximately four in five drinkers would reduce their risk of death from any causes ifthey cut their alcohol intake by one unit (10 grams) per week.
- Measures of the health benefits and harms associated with alcohol use may need to
- Life years potentially gained, quality of life and individual preferences over the timing ofoutcomes are important elements in the analysis of policy options.
- Alcohol policies have to balance welfare benefits and losses. Harms to people other than drinkers are more effectively reduced by tackling heavy drinking. Price and regulation policies are more likely to affect consumer welfare.
- Harms to others, addiction, and consumers’ inaccurate perception of risk provide strong justification for government action in addressing the problem of harmful alcohol use.
03 de juny 2015
An open mind on mental health
Fit mind, fit job. From Evidence to Practice in Mental Health and Work
The social and economic impact of mental illness requires a new approach. Conventional approaches to the disease are insufficient and a broad involvement of different stakeholders is needed. These are the premises that the OECD has drawn in its new report "Fit mind, job fit. From evidence to practice in mental health and work. " While in previous reports had tried to characterize the state of affairs, now he has been concerned to review successful strategies in different countries.
The total costs of mental illness represent around 3.5% of GDP in European countries. Of this, more than half corresponds to indirect and intangible costs. Among them are productivity losses, an aspect difficult to estimate because the phenomenon of "presenteeism" appears. In the case of mental illness, the fact of going to work despite illness is the rule (over 75%) .
The issue presents differential considerations for other diseases, especially its relationship with the job and productivity. There is evidence of less satisfaction, lower quality jobs and lower pay. All contribute to conditions of work under a mental illness represent a tension for the individual and for the company. And of course in the event of unemployment, even more.
Ssome countries have tried to deal with this situation from an interdisciplinary way. That is, strictly avoiding medicalized view of health policy and trying to involve the various actors in the field of business and social environment of the patient.
The OECD recommendations fall into four areas: youth and education, business, social services and employment and healthcare. Of these, I would like to highlight here those related to the firm, being the most neglected at present.
In the field of business, strategies for supporting employees with mental health problems are crucial to achieve a positive development that avoids the end a loss of jobs and a worsening of the disease. The initial issue to consider is the detection of the problem. Somehow, managers and immediate supervisors need to provide a suitable response to the situation and often do not have the knowledge and training needed. The British example known as "Mental Health First Aid program" is a tipping point to keep in mind despite his limited success in small and medium enterprises.
The adoption of risk prevention strategies also seeks to provide tools to improve psychosocial job conditions. To this, a change of perspective in occupational medicine could contribute decisively.In cases of injury, the management of return to work eventually becomes critical for improving the stage of the disease process. To the extent that the long absences are more complex to address, it is precisely these that require attention consistently. The option of gradual return to work and support by colleagues has proven effective in this regard. The search for a negotiated solution brings more satisfactory exit routes for the disease, the conflict. And finally there are the incentive strategies and the legal obligations of employers in this regard. How to address long-term absenteeism it is a challenge in all countries and there is no rècipe for all cases. Must be combined with adequate monitoring incentives to return to the job.The uniqueness of mental illness is that the successful approach is the one that allows redevelopment activities in the labor and social environment properly. To do this, a modern approach requires among other things that the company and its employees are aware of and responsible for a different perspective and fully involved. In this direction, government and business associations should join hands to tackle an issue that so far we thought belonged only to the health system. The relevance of mental health and its impact on the welfare of citizens and their families, requires a timely response.
The social and economic impact of mental illness requires a new approach. Conventional approaches to the disease are insufficient and a broad involvement of different stakeholders is needed. These are the premises that the OECD has drawn in its new report "Fit mind, job fit. From evidence to practice in mental health and work. " While in previous reports had tried to characterize the state of affairs, now he has been concerned to review successful strategies in different countries.
The total costs of mental illness represent around 3.5% of GDP in European countries. Of this, more than half corresponds to indirect and intangible costs. Among them are productivity losses, an aspect difficult to estimate because the phenomenon of "presenteeism" appears. In the case of mental illness, the fact of going to work despite illness is the rule (over 75%) .
The issue presents differential considerations for other diseases, especially its relationship with the job and productivity. There is evidence of less satisfaction, lower quality jobs and lower pay. All contribute to conditions of work under a mental illness represent a tension for the individual and for the company. And of course in the event of unemployment, even more.
Ssome countries have tried to deal with this situation from an interdisciplinary way. That is, strictly avoiding medicalized view of health policy and trying to involve the various actors in the field of business and social environment of the patient.
The OECD recommendations fall into four areas: youth and education, business, social services and employment and healthcare. Of these, I would like to highlight here those related to the firm, being the most neglected at present.
In the field of business, strategies for supporting employees with mental health problems are crucial to achieve a positive development that avoids the end a loss of jobs and a worsening of the disease. The initial issue to consider is the detection of the problem. Somehow, managers and immediate supervisors need to provide a suitable response to the situation and often do not have the knowledge and training needed. The British example known as "Mental Health First Aid program" is a tipping point to keep in mind despite his limited success in small and medium enterprises.
The adoption of risk prevention strategies also seeks to provide tools to improve psychosocial job conditions. To this, a change of perspective in occupational medicine could contribute decisively.In cases of injury, the management of return to work eventually becomes critical for improving the stage of the disease process. To the extent that the long absences are more complex to address, it is precisely these that require attention consistently. The option of gradual return to work and support by colleagues has proven effective in this regard. The search for a negotiated solution brings more satisfactory exit routes for the disease, the conflict. And finally there are the incentive strategies and the legal obligations of employers in this regard. How to address long-term absenteeism it is a challenge in all countries and there is no rècipe for all cases. Must be combined with adequate monitoring incentives to return to the job.The uniqueness of mental illness is that the successful approach is the one that allows redevelopment activities in the labor and social environment properly. To do this, a modern approach requires among other things that the company and its employees are aware of and responsible for a different perspective and fully involved. In this direction, government and business associations should join hands to tackle an issue that so far we thought belonged only to the health system. The relevance of mental health and its impact on the welfare of citizens and their families, requires a timely response.